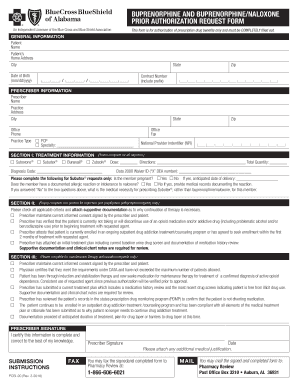
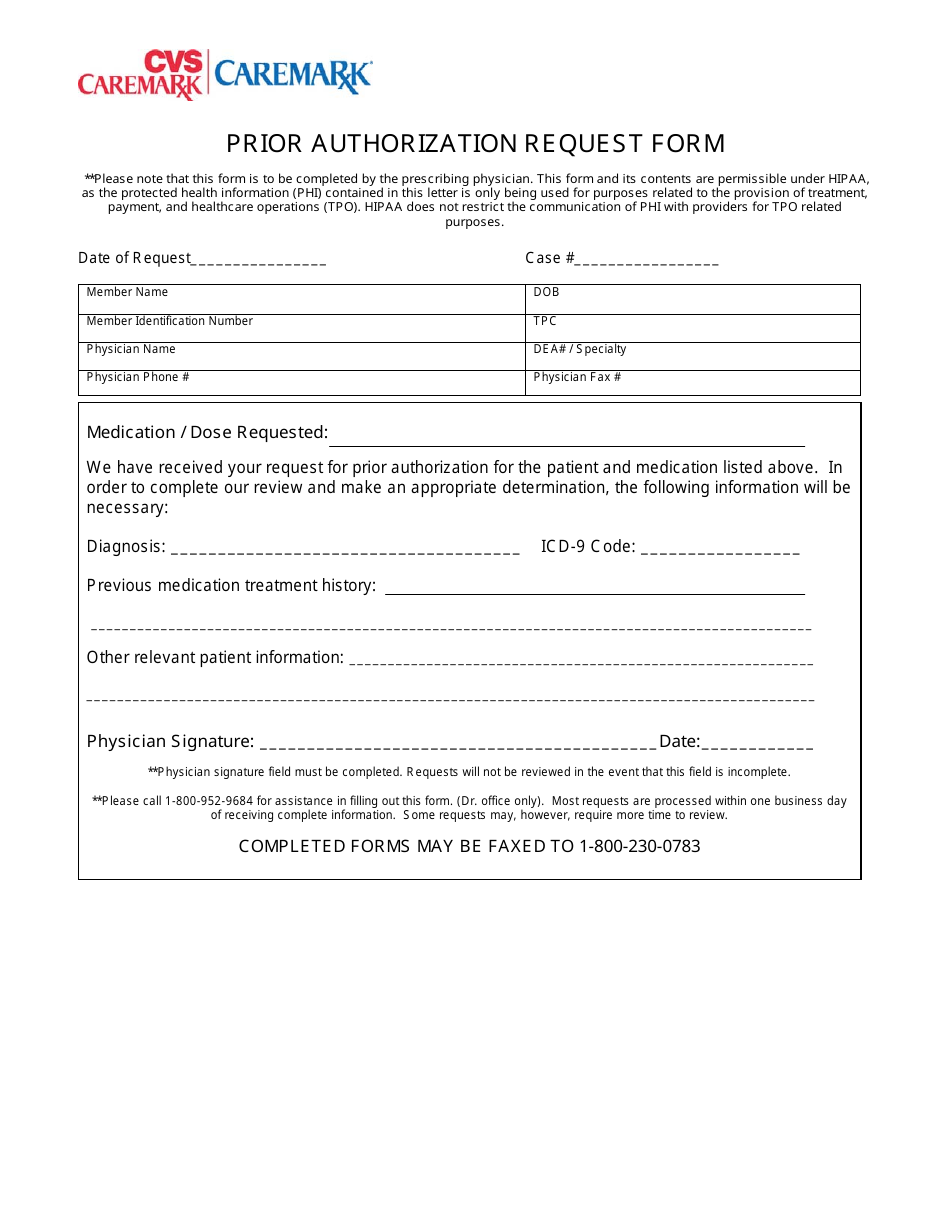
This means that you will need to get approval from Health First Health Plans before you fill your prescriptions. Complete the Prior Authorization form.
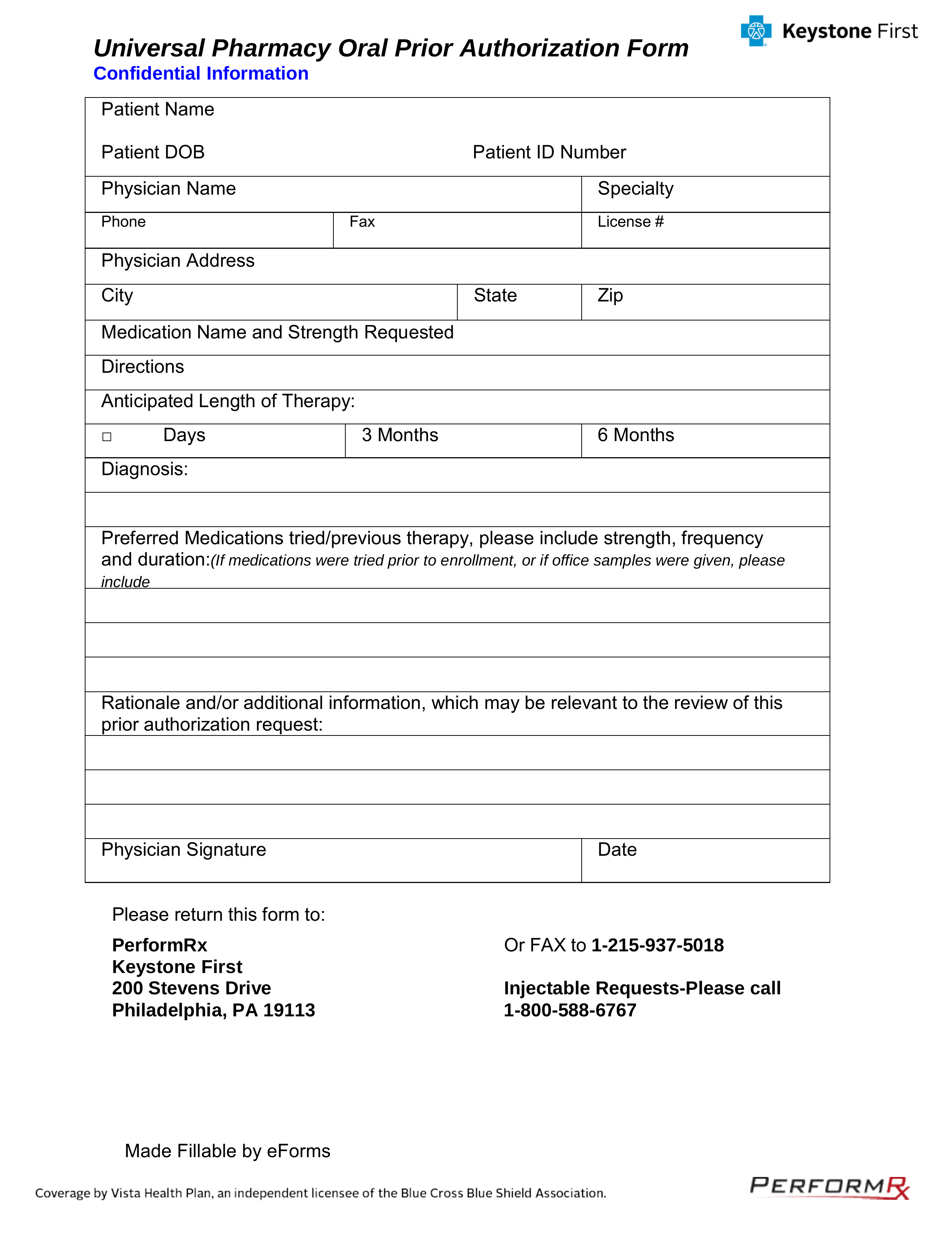 Free Keystone First Rx Prior Authorization Form Pdf Eforms
Free Keystone First Rx Prior Authorization Form Pdf Eforms
Since coverage will not be authorized without it beginning the prior authorization process early is important.

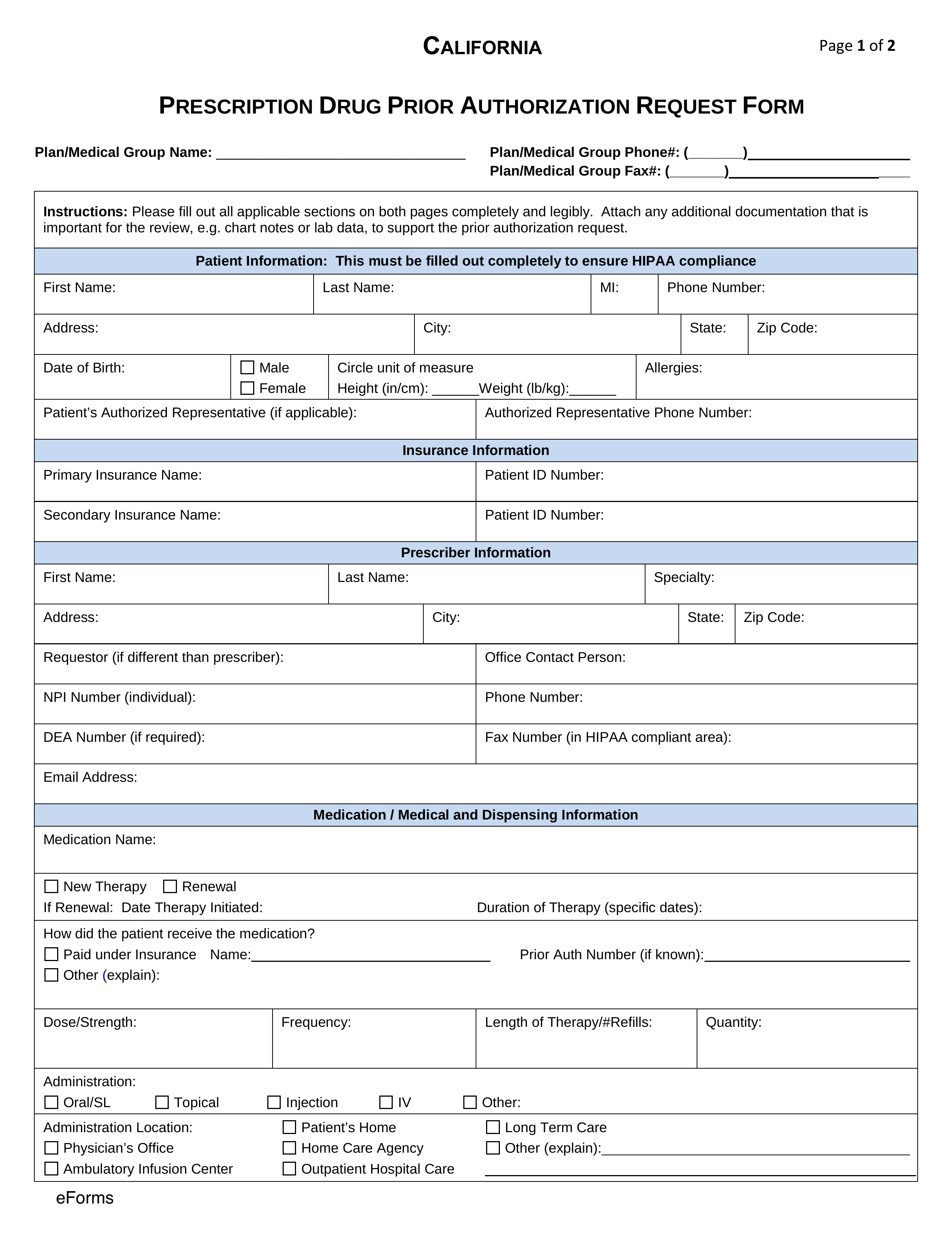
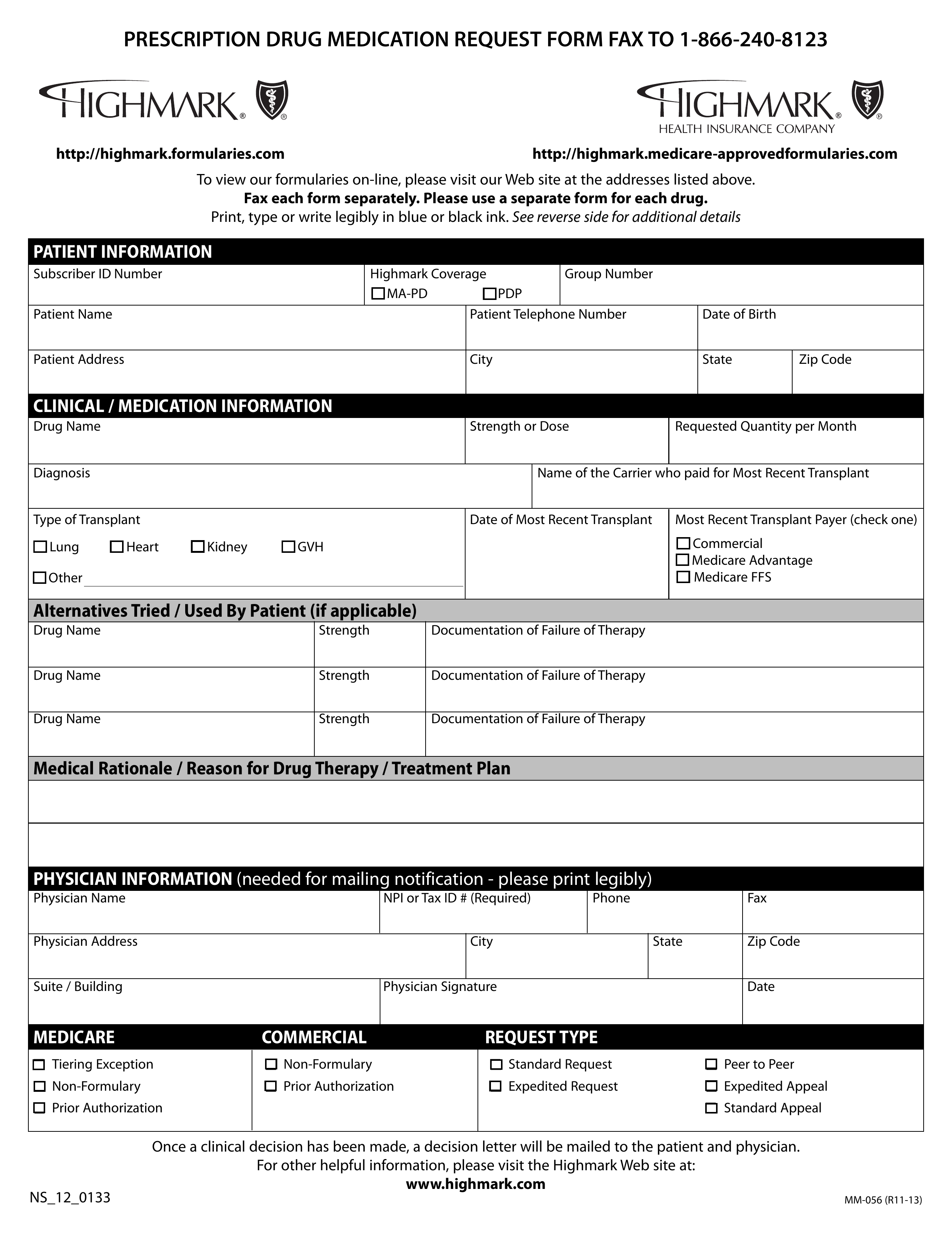
First health prior authorization. Your non-participating provider may obtain prior authorization for you or your authorized representative by calling 1-855-281-1840 TTY 711. Providers should fax the completed FFS Prior Authorization Request Form as the coversheet for the supporting documentation they are submitting with the request. What is a Prior Authorization.
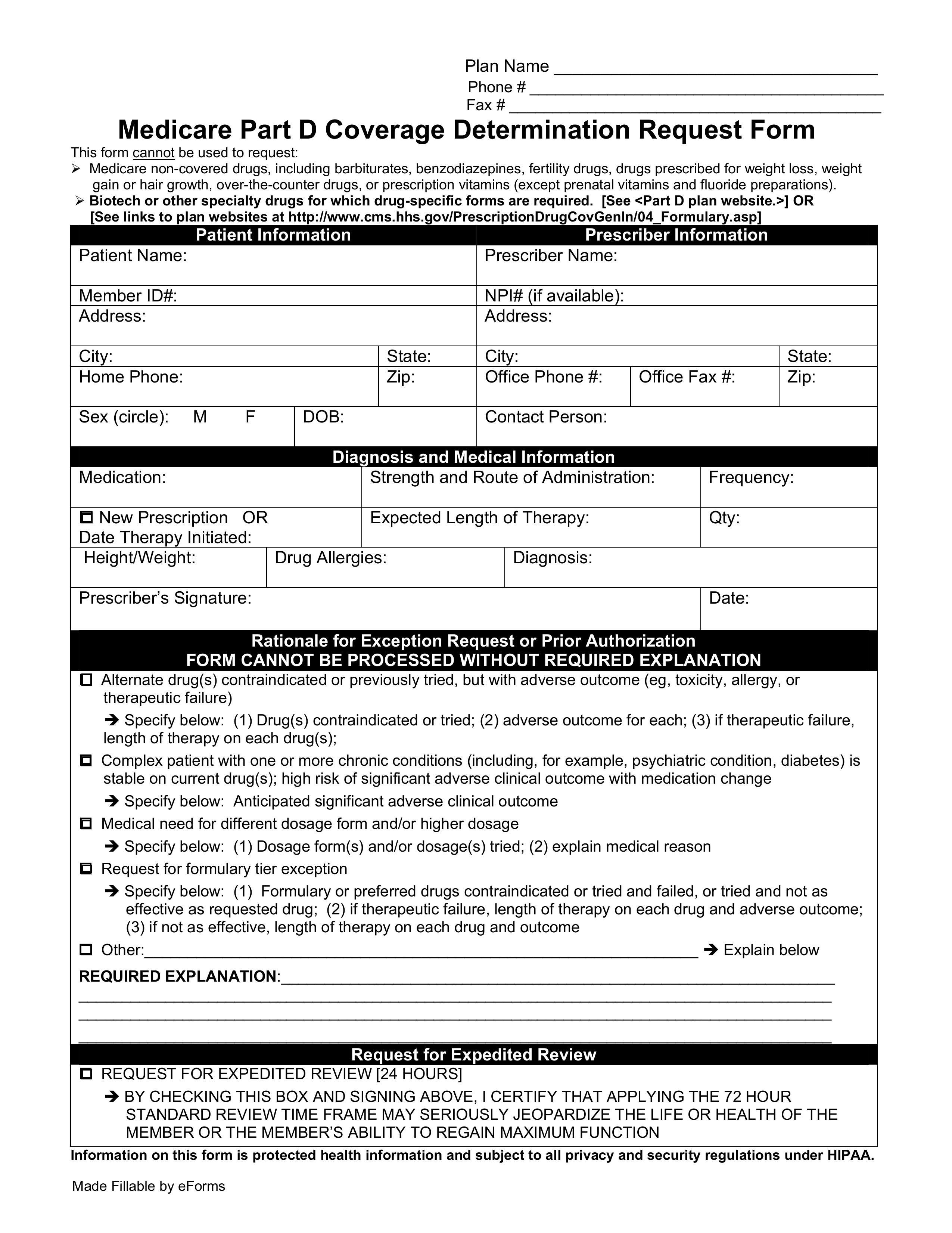
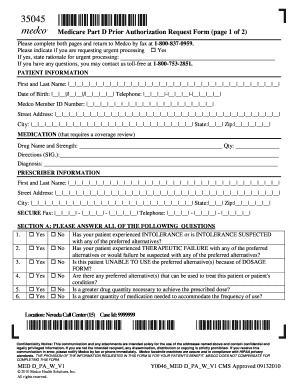
An Issuer may also provide an electronic version of this form on its website that you can complete and submit electronically through the issuers portal to request prior authorization of a health care service. The penalty does not apply toward your deductible or out-of-pocket maximum so it is. Prior authorization is usually required if you need a complex treatment or prescription.
Providers must receive prior approval before delivering services in order to be eligible for payment. Prior Approvals for the Mental Wellness and Counselling Program the Missing Murdered Indigenous Women Girls Health Support Services Program. A prior authorization PA sometimes referred to as a pre-authorization is a requirement from your health insurance company that your doctor obtain approval from your plan before it will cover the costs of a specific medicine medical device or procedure.
Health First Health Plans does not discriminate on the basis of race color national origin disability age sex gender identity sexual orientation or health status in the. Date of requested service _ Days Visits Requested. Members with Medicaid as a secondary payer.
To simplify your experience with prior authorization and save time please submit your prior authorization request through the following online portals. This pre-authorization request form should be filled out by the provider. Prior Authorization Requests PARs or Admission Reviews - Hospitals will be submitting based on established timelines before or shortly after admission for all services excluding the following Maternity and maternity.
2021 Prior Authorization Criteria Health First Commercial Plans Inc. Prior authorization is needed for diagnostic testing out-patient procedures non-emergency hospitalizations surgeries infusions and high cost specialty injectable medications etc in accordance with the list located in the Summary Plan Document. Admissions to long term rehabilitation facilities.
All requested data must be provided. Effective April 3 2020 Health First Colorado is waiving prior authorization requirements for oxygen therapy positive airway pressure devices respiratory assist devices ventilators suction devices nebulizers and oxygen-related supplies that are emergently provided for COVID-19 treatment. Is doing business under the name of Health First Health Plans.
How do I receive prior authorization. Health First Health Plans requires you or your physician to get prior authorization for certain drugs. Fax it with clinical documentation and completed Preadmission Screening and Resident Review PASRR to our prior authorization fax line at 1-860-860-8056 for review.
If you dont get approval Health First Health. For custodial requests we need the actual date of admission and prior coverage payer information. All emergency or urgent admissions are subject to.
Electronic Prior Authorization ePA Submit an ePA using CoverMyMeds. All mandatory fields on the form must be completed accurately in order to avoid delays in receipt and processing of. If you dont obtain prior authorization for services in the non-participating provider network you may have to pay the entire expense.
Capitated behavioral health services. If you require a RUSH Prior Authorization for a procedure being done within 48 hours please call Moda Health at 503 243-4496 or 800 258-2037 fax 503 243-5105 or toll free fax 800 522-7004 Referral Standard Retro Urgent Could seriously jeopardize the life or health. Only providers who are registered with the Health Benefits Program can request prior approval for counselling services.
Benefits for services received are subject to eligibility and plan terms and conditions that are in place at the time services are provided. In the case of emergencies or urgent situations a retrospective prior authorization will be carried out. Ask your doctor if a prescription medication is going to require prior authorization so.
PCP Phone _PCP Fax Diagnosis. Use this form to request authorization by fax or mail when a n issuer requires prior authorization of a health care service. Fax completed prior authorization request form to 877-309-8077 or submit Electronic Prior Authorization through CoverMyMeds or SureScripts.
The Fee For Service FFS Prior Authorization Request Form is to be completed by registered providers to request an authorization. Before completing this form please confirm the patients benefits and eligibility.