UTILIZATION MANAGEMENT PLAN Page. Supply Utilization Management helps reducing wastages value mismatch and misuse through standardization and proper specification.
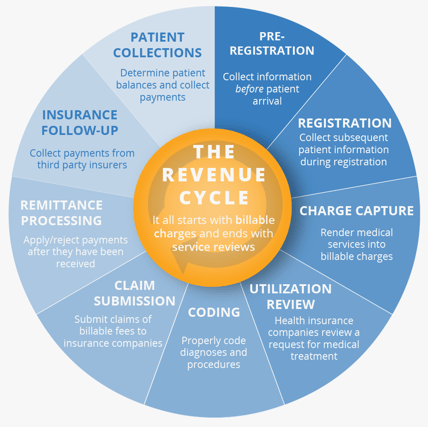 The 9 Steps Of Healthcare Revenue Cycle Management Explained
The 9 Steps Of Healthcare Revenue Cycle Management Explained
UTILIZATION MANAGEMENT PROGRAM DESCRIPTION MEDICAL ASSOCIATES HEALTH PLANS 2018 AUTHORITY Medical Associates Health Plan Inc.
Utilization management in healthcare pdf. Utilization Management Program 2014 Molina Healthcare MedicaidHealthy Michigan Plan Manual Page 5 of 16 Fax your authorization request and clinical information if required to the UM Department at 800-594-7404. Health Partners Plans Provider Manual Utiliz ation Management - February 2014 Page 7-1 Purpose. Medical Health Team a.
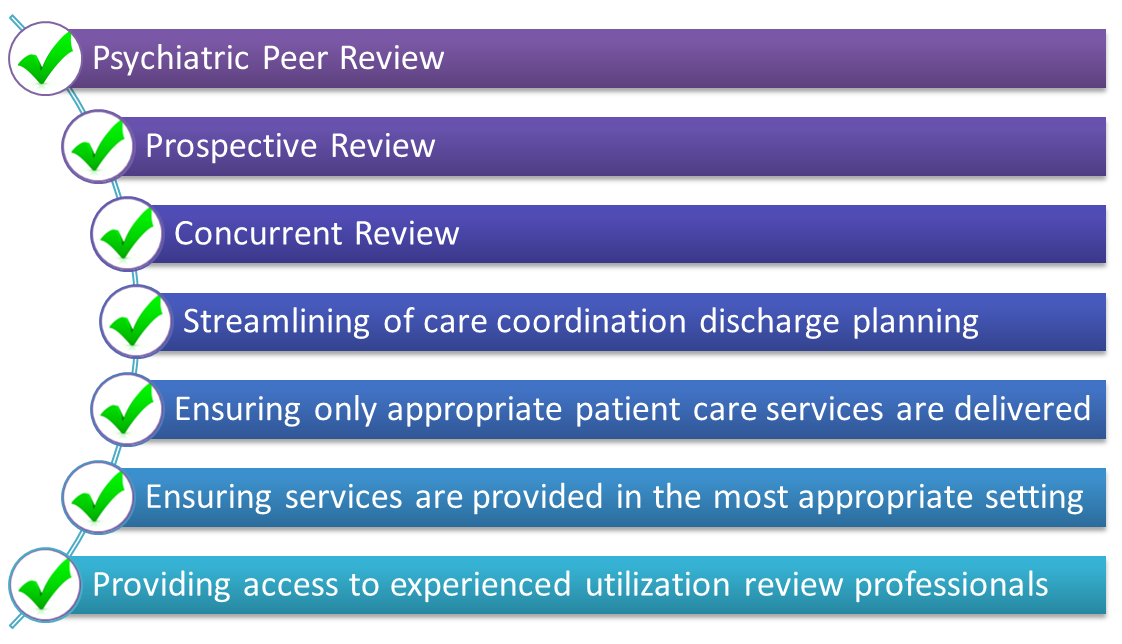
Requests for services are reviewed by Masters-level behavioral health clinicians andor psychiatrists. This process is run by or on behalf of purchasers of medical services ie insurance providers rather than by doctors. Utilization management clinicians practice at peak productivity while healthcare organizations and providers work more efficiently and cost effectively.
Case Managers Social Workers 2. Utilization Management Section H. Virtual centralization of the supply chain on the other hand helps improving level of cooperation in hospitals thereby helping them controlling costs and improving services.
2 any other entity or organization in which Tenet Healthcare Corporation or an Affiliate. Whether it be a solid or dotted line to Finance these teams must work together to ensure the financial. 03 -19 15 Previous Versions Dated.
AbstractUtilization management encompasses a diverse set of activities designed to influence the use of health care services and thereby constrain health care resource consumption. And Medical Associates Clinic Health Plan of Wisconsin collectively doing business as Medical Associates Health Plans and hereafter referred to as MAHP have entered into contractual relationships or services agreements to make provision for. Now that Utilization Management department activities increasingly influence reimbursement and affect revenue there is a move towards re-organizing or realigning Utilization Management to the finance function.
Utilization Management is an integral part of the US healthcare ecosystem used by health insurers or Pharmacy Benefit Managers PBMs to evaluate the appropriateness medical necessity and efficiency of healthcare services rendered to patients. Improve the quality of service at the right cost in the right setting. Utilization management UM is a process that evaluates the efficiency appropriateness and medical necessity of the treatments services procedures and facilities provided to patients on a case-by-case basis.
Utilization Management RNs e. Robotics Utilization for Healthcare Digitization in Global COVID-19 Management Zeashan Hameed Khan 1 Afifa Siddique 2 and Chang Won Lee 3 1 Department of Mechatronics and Biomedical Engineering Air University Islamabad 44000 Pakistan 2 Pakistan Institute of Medical Sciences PIMS Islamabad 44000 Pakistan. Utilization management UM is now an integral part of most public and private health plans.
Physician Reviewers MD c. Bailit and Cary Sennett. Aetna Better Health together with its affiliates has more than 25 years of experience in effectively and efficiently.
These reductions appear to have had limited impact on aggregate health. NCQA Definition of Utilization management. Behavioral Health Utilization Management Social Workers e.
Utilization management as a cost-containment strategy by Howard L. Utilization management UM is the evaluation of the medical necessity appropriateness and efficiency of the use of health care services procedures and facilities under the provisions of the applicable health benefits plan sometimes called utilization review IOMs Committee on Utilization Management by Third Parties 1989 A set of techniques used by or on behalf of purchasers of. Eemer 4 2019.
Utilization Management aims to. Evaluating determining coverage for and appropriateness of medical behavioral health care services as well as providing needed assistance to providers and patients in cooperation with other parties to ensure appropriate use of resources. Utilization Management Considerations for Care Management Entities 1 number of states and regions have begun to demonstrate cost savings and improved clinical and functional outcomes for youth with severe behavioral health needs through a Care Management Entity CME approach1 CMEs provide accountable care for children with behavioral health needs who.
Medical Director of Care Management MD FMOB b. Care Management Manager RN BSN CCM d. Case Managers RNs and Social Workers UM Staff apply evidence.
Hospital review until recently the primary focus of UM is associated with a reduction in bed days and rate of hospital cost increases. 05-12-16 Retires Policy Dated. In this report the committee considers utilization management as a set of techniques used by or on behalf of purchasers of health care benefits to manage health care costs by influencing patient care decision-making through case-by-case assessments of the appropriateness of care prior to its provision.
Originally utilization management in healthcare started with a narrow focus. This policy applies to 1 Tenet Healthcare Corporation and its wholly-owned subsidiaries and affiliates each an Affiliate. If a requested.
How virtual centralization works is explained with the help of an example of CSC. Care Management Associates f. This chapter provides an introduction to Health Partners Plans Utilization Management team and the guidelines and criteria used by the department to achieve optimal benefit utilization for our members.
1 of 19 Effective Date. Healthcare organizations conduct utilization management activities only for those services admissions and continued stays where there is ROI for conducting the review. PCPsSpecialists should use the Molina Healthcare Service Request Form or the Michigan Healthcare Referral Form.
Utilization Management UM Section 8 of RFP H1 Describe how you will ensure that services are not arbitrarily or inappropriately denied or reduced in amount duration or scope as specified in the Louisiana Medicaid State Plan.