Submit online at Express Scripts or call 1-800-935-6103. Review your request statusdecision online.
 Blue Cross Blue Shield Prior Authorization Form Florida Fill Online Printable Fillable Blank Pdffiller
Blue Cross Blue Shield Prior Authorization Form Florida Fill Online Printable Fillable Blank Pdffiller
Thank you for browsing our provider forms.
Bcbs of oklahoma prior authorization form. The Oklahoma Medicaid prior authorization form is a document which is employed by a medical office in order to request Medicaid coverage for a drug which is not on the States Preferred Drug List PDL. Many times your doctor will need to get approval prior authorization before your plan will cover certain health care services and medicines. When you know what steps you need to take before treatment things go more smoothlyOne of the most important steps is prior authorization.
405 522-6205 option 6. 1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross. If you have any questions or comments about the forms please contact us.
Direct Deposit Request Form. View Part D prior authorization requirements. Contact Provider Services at 1-866-518-8448 for forms that are not listed.
GENERAL INFORMATION Patient Name Request. We have provided a downloadable PDF version of this form on this webpage. Appeal submission with authorization - Resolve billing issues that directly impact payment or a write-off amountNote the different fax numbers for clinical vs.
Standard Authorization Form and other HIPAA Privacy Forms Authorizes Blue Cross and Blue Shield of Oklahoma to disclose protected health information only to those individuals specified by the member. Managed Care Referral Form. Blue Cross Blue Shield of Wyoming 8004247094.
All NC Providers must provide their 5-digit Blue Cross Blue Shield of North Carolina Blue Cross NC provider ID below. Incomplete forms may delay processing. Carewise audit appeals should go directly to Carewise as noted in the letter sent to providers.
Documents and Forms-----Language Assistance. For pharmacy call customer service for pharmacy benefit drugs. Blue Cross and Blue Shield of North Carolina.
Request Forms Prior Authorization Request Form Online Prior Authorization Form. Horizon Blue Cross Blue Shield of New Jersey 8003911926. Review the prior authorizationstep therapy program overview list to help you determine which prior authorization form is used for the medication being prescribed.
Medicaid in the State of Oklahoma is provided by Soonercare which is funded jointly by the. 15 rows Deductible Credit Form for Employees at Enrollment. If you have questions or concerns regarding these programs please call Prime Therapeutics at 800-991-5643.
There are important changes to the preauthorization requirements for some of your Blue Cross and Blue Shield of Oklahoma BCBSOK patients. Understanding your health insurance is the best way to enjoy all its benefits. October 10 2019.
Coordination of BenefitsBlue Cross and Blue Shield of Alabama is Host Plan. An Independent Licensee of the Blue Cross and Blue Shield Association MKT-148 Rev. CoverMyMeds automates the prior authorization PA process making it the fastest and easiest way to review complete and track PA requests.
1 2020 preauthorization will be required or expanded for. Prior Authorization and Step Therapy Programs. Step Therapy Program Criteria Summary and Fax Form List.
Prior Review and Limitations Prior Authorization Facsimile Form Online Prior Authorization Requests. 12 rows Disabled Dependent Authorization Form for Individual Plans. CoverMyMeds is BlueCross BlueShield of Oklahoma Prior Authorization Formss Preferred Method for Receiving ePA Requests.
Blue Cross and Blue Shield of Oklahoma 8773530992. Member authorization is embedded in the form for providers submitting on a. Medical Authorization Unit - for current status of requested services documentation requirements per type of requested service and the need for urgent authorization of services.
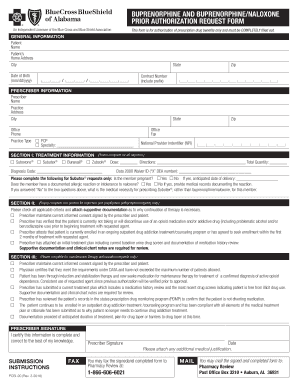
5-2016 SUBMISSION INSTRUCTIONS GENERAL PRESCRIPTION DRUG COVERAGE AUTHORIZATION REQUEST FORM This form is for authorization of prescription drug benefits only and must be COMPLETELY filled out. You can sign up to use the electronic prior authorization ePA system through CoverMyMeds all that is needed is a computer and an internet connection. Northwood DMEPOS Management Program Procedure Codes Requiring Prior Authorization PDF Patient eligibility precertification and preauthorization contacts.
Once a request is submitted you can visit HealtheNet to check the status of a prior authorization. Select the appropriate BlueCross BlueShield of Oklahoma form to get started. AUTHORIZATION REQUEST Submission of this form is only a request for services and does not guarantee approval.
Blue Cross and Blue Shield of Oklahoma. Outpatient provider administered drug therapies including Cellular Immunotherapy Gene Therapy and other. 800 522-0114 option 6.
Prior Authorization Forms Select pharmacy tab Prior Authorization Request Form Online Prior Authorization Form. Protected health information is defined by privacy rules enacted under the Health Insurance Portability and Accountability Act HIPAA of 1996. 405 702-9080 local statewide 1-866-574-4991.
15 rows Standard Authorization Form and other HIPAA Privacy Forms Authorizes.
