Utilization Management and Quality Assurance 18 Primary Care Physician Responsibilities 20 Case Management 22 Notifications 25 Appendix I. -Eliminate unnecessary services -Maximize savings to your health plan Healthcare services are evaluated for medical necessity appropriateness and.
 Utilization Management Quality Improvement In Healthcare Study Com
Utilization Management Quality Improvement In Healthcare Study Com
BACKGROUND OF THE STUDY.
Utilization management organization. A government-run insurance program for low income people. People and Entities Involved in Utilization Management Medicare. Kepros Utilization Management UM program promotes quality and cost-effective healthcare and member well-being that ensures appropriate utilization of services.
A government-run insurance program for people 65 and older. Balanced against these forces are several threats posed by evaluation. It is a way of getting improved results in managerial action.
Prior to initiating any review procedures the utilization management organization should provide in writing its name address telephone number organizational structure contact person Medical director review procedure nature of their informed consent procedures and appeal process. Management by objectives can be. Utilization Management Program Description 4 Organizational Structure Responsibility 9 Utilization Management Committee Description 12 Evaluation of the Utilization Program 14 Delegation 15 Interface.
Management by objectives is one of such tools. Telligens Utilization Management program makes sure your members get the evidence-based medical care they need. NCQA Utilization Management Accreditation helps guarantee that organizations making these decisions are following objective evidence-based best practices.
The Utilization Management department can help with managing the cost and delivery of services. Also clients of utilization management organizations have a strong interest in obtaining reports on results and in shifting their business to other firms if they cannot get such reports. AbstractUtilization management encompasses a diverse set of activities designed to influence the use of health care services and thereby constrain health care resource consumption.
Quality of Care Review System and Organization. The Board of Management is authorized with the consent of the Supervisory Board to exclude subscription rights of shareholders from capital increases in form of cash contributions in the course of one-time or multiple utilizations of Authorized Capital II up to an amount not exceeding 10 percent of the capital stock during the timeframe of the effective date of the authorization and the date of utilization. The members of the Committee are appointed by the Chief Medical Officer report to the.
An example of managed care. It involves a prospective review of. The Utilization Management Committee UMC is delegated by the Clinic Board of Directors to carry out utilization management duties.
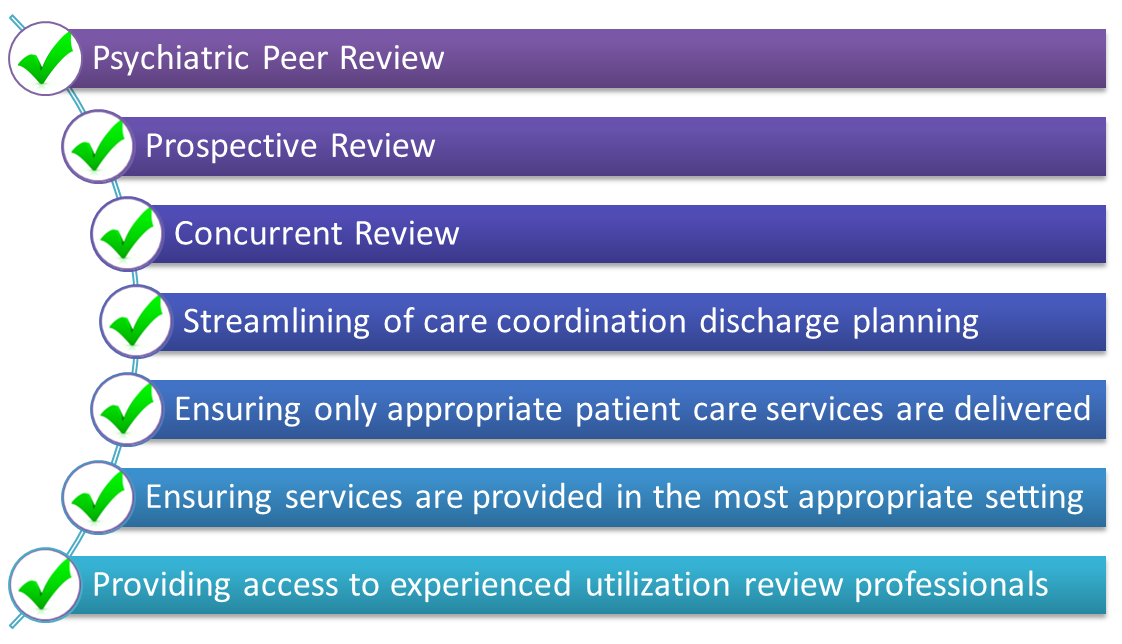
Utilization management helps ensure that patients have the proper care and the required services without overusing resources. Telligens utilization management program is designed to. -Ensure high quality care is delivered to those who medically need it.
Utilization management UM is the evaluation of the medical necessity appropriateness and efficiency of the use of health care services procedures and facilities under the provisions of the applicable health benefits plan sometimes called utilization review. Utilization Management UM initially referred to as Utilization Review UR remains a well-recognized component of a cost management approach in the health care service delivery and payment arenas. UM processes include interventions that take place.
The integration of the Utilization Management department and its processes within hospital operations can increase care efficiency and decrease revenue loss. Effective Utilization Of Management By Objectives In Nigerian Organization. For example reviewing for medical necessity is one of the various utilization management processes.
We currently provide UM in eight states and bring broad knowledge and industry-best practices to maximize quality care and cost-effective outcomes across the continuum of care. Utilization management the plans of care developed by child and family teams drive medical necessity with the MCOs role shifting to management of outlier utilization. Management needs a lot of tools to be able to administer effectively in the day to day running of the business.
They are health insurance companies that. Prefered Provider Organization PPOs. Approaches for the implementation of utilization management activities in CMEs can vary considerably.
