A committee will then decide. Persons covered under a UnitedHealthcare.
 United Healthcare Appeal Form 2018 Beautiful United Healthcare Medication Prior Authorization Form Pdf 10 Humana Models Form Ideas
United Healthcare Appeal Form 2018 Beautiful United Healthcare Medication Prior Authorization Form Pdf 10 Humana Models Form Ideas
Prior Rx Authorization Forms Prescription prior authorization forms are used by physicians who wish to request insurance coverage for non-preferred prescriptions.
Unitedhealthcare medical drugs prior authorization form. All mandatory fields on the form must be completed accurately in order to avoid. You may also initiate your request by phone by calling the. In some cases a patient might need treatment that is not covered by their health care plan.
UnitedHealthcare is an operating division of UnitedHealth Group the largest single health carrier in. Commercial Prescription Prior Authorization Form - Arkansas Iowa Mississippi Oklahoma West Virginia. More forms can be found in the Clinical Pharmacy and Specialty Drugs Prior Authorization Programs section.
Adding prior authorization and site of care. Please submit your request online using our Prior Authorization and Notification tool on Link. Medicaid recommends that providers prescribe medications on their Preferred Medication List PDL but in the event that a particular drug is not on this list a Mississippi Medicaid prior authorization form can be completed by the prescribing physician to order this particular medication.
You may also initiate your request by phone by calling the number on the back of the members health plan ID card. Prior Authorization Request Form Medica requires that providers obtain prior authorization before rendering services. Medical Drugs Prior Authorization Form You may use this form to request prior authorization for medical drugs.
This form may contain multiple pages. At UnitedHealthcare we are committed to improving the health care system. They must then wait to receive a decision before they can perform the Medicare services in question or prescribe the prescription drug being considered.
The purpose of this form is to demonstrate medical justification for prescribing the drug in question when other drugs on the PDL might serve the same purpose. We will expand the prior authorization requirement to all outpatient places of service for all drugs in the class. If you have questions please call 800-310-6826.
Prior Authorization Request Form Please complete this entire form and fax it to. For forms to request prior authorization for drugs covered under the retail pharmacy benefit please visit the OptumRx Healthcare Professionals Portal. Standalone personal representative form pdf These optional forms are used by the member to provide UnitedHealthcare with authorization to discuss their claim with someone other than the member.
Commercial Prescription Prior Authorization Form. Please use the forms below to request prior authorization for drugs covered under the medical benefit. UnitedHealthcares home for Care Provider information with 247 access to Link self-service tools medical policies news bulletins and great resources to support administrative tasks including eligibility claims and prior authorizations.
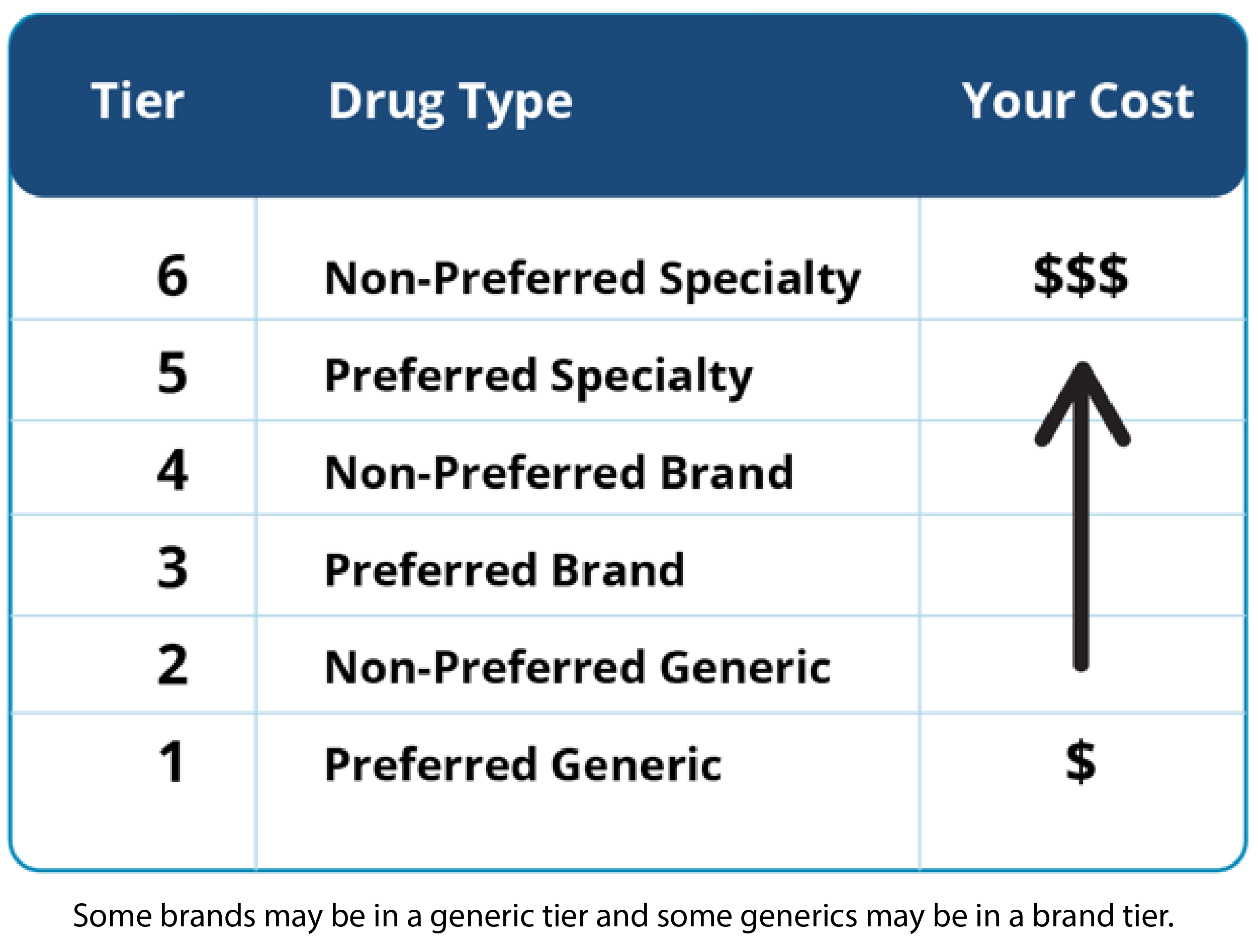
The Fee For Service FFS Prior Authorization Request Form is to be completed by registered providers to request an authorization. Allow at least 24 hours for review. A non-preferred drug is a drug that is not listed on the Preferred Drug List PDL of a given insurance provider or State.
Not for members living in New York. Prior authorization works by having your health care provider or supplier submit a prior authorization form to their Medicare Administrator Contractor MAC. Please complete all pages to avoid a delay in our decision.
This class currently requires notificationprior authorization including site of care reviews. Complete this form to request a formulary exception tiering exception prior authorization or reimbursement. When you find the plan you may want to enroll in click the View Plan Details button to access your enrollment form.
Member Information Prescriber Information Member Name. The forms below cover requests for exceptions prior authorizations and appeals. Providers should fax the completed FFS Prior Authorization Request Form as the coversheet for the supporting documentation they are submitting with the request.
Standalone Direct Deposit form pdf Note. Medicare Prescription Drug Coverage Determination Request Form PDF 38704 KB Updated 121719 For use by members and providers. If any items on the Medica Prior Authorization list are submitted for payment without obtaining a prior authorization the related claim or claims will be denied as provider liability.
Most services including prescription drugs are covered by Home State Health MissouriCare and UnitedHealthCare. These paper fax forms are meant to be used in requesting prior authorizations for specific drugs for the state of Virginia Community Plan care providers. Peer to Peer Scheduling Request Form - UnitedHealthcare offers the opportunity for your physician to speak with our medical director to discuss the medical policy and documentation requirements which determined the response for your prior authorization.
Providers prescribing medication not covered by their patients health care plan must submit a Missouri Medicaid prior authorization form. The form should be submitted to UHC where they will review the physicians medical. The provider will have 60 days from the date of the claim denial to appeal and.
In some cases a physician may choose to prescribe medication that is not on the preferred drug list PDL and will have to fill out a UnitedHealthcare prior authorization form. This application form is used to ensure that the patient in question is receiving the. Standard Prior Authorization Request Form Please submit your request online using our Prior Authorization and Notification tool on Link.