Below is the list of specific services in these categories that require precertification. Procedures Tests Services Requiring Preauthorization CPTHCPCS codes Preauthorization Method Responsible Provider ClinicalCriteria Source Acute Inpatient Rehabilitation Level of Care NA BCBSRI Traditional Rendering BCBSRI Policy Ambulance Air and Water A0430 A0431 A0435 A0436 BCBSRI Traditional Rendering BCBSRI Policy Anastomosis of Extracranial-Intracranial Arteries 61711 MHK.
Https Www Empireblue Com Provider Noapplication F3 S2 T2 Pw Ad067834 Pdf Refer Ehpprovider
Administrative Services Only ASO Plans.
Bcbs prior authorization. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. An in-network health care provider will request a prior authorization on your behalf. 1 2021 Blue Cross and Blue Shield of Texas BCBSTX will update its list of Current Procedural Terminology CPT codes requiring prior authorization to comply with changes as a result of new replaced or removed codes implemented by the American Medical Association AMA and BCBSTX.
If we determine that the services are medically necessary we send an approvalor authorizationin writing to the member primary care provider PCP the treating physician and the facility if applicable to let them know that we have approved the services. Massachusetts Standard Form for Medication Prior Authorization Requests eForm or contact Clinical Pharmacy Operations. Prior authorization forms Download and print the most commonly requested prior authorization fax forms for procedures injectable drugs office administered and home self-administered and oraltopical drugs choosing from the lists below.
Who requests prior authorization. Request preauthorization Preauthorization allows us to review and determine the medical necessity of a service drug andor the appropriateness of the setting. This list will be updated no more than twice a calendar year.
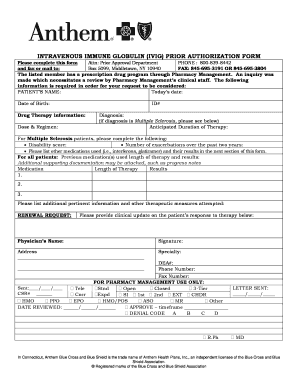
Usually the provider is responsible for requesting prior authorization before performing a service if the member is seeing an in-network provider. Some services require prior authorization before they are performed. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required.
Information for Blue Cross and Blue Shield of Illinois BCBSIL members is found on our member site. Medical Policy and Pre-certificationPre-authorization for Out-of-Area Members Whats New. 19318 REDUCTION OF LARGE BREAST Pre-operative evaluation height weight previous.
Most preauthorization requests can be resolved by contacting Provider Relations and Servicing or. Prior Authorization Services for. Blue Shield may require additional information after the service is provided.
Prior authorization requirements apply to all of the HealthSelect plans except HealthSelect SM Secondary. Northwood DMEPOS Management Program Procedure Codes Requiring Prior Authorization PDF Patient eligibility precertification and preauthorization contacts Medical policy precertification and preauthorization router. While the list below covers the medical services drugs and procedures that require authorization prior to rendering.
For dates of service on or after Jan. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. Prior Authorizations BCBSTX must approve certain covered health services before you get them.
When a request for service is not approved we notify the PCP and the member. However out-of-network providers are not contracted with us and have not agreed to accept this responsibility. Blue Choice members using their self-referred benefit do not need to get prior authorization.
Sometimes a plan may require the member to request prior authorization for services. Preauthorization is required or recommended based on the plan for a number of services and drugs as noted in our policies. Other medications that require prior authorization.
Members and providers are encouraged to obtain prior authorization and may call Customer Service to inquire about the need for prior authorization. Obtaining a preauthorization helps us pay claims faster with no denied charges or unexpected costs to our members. Require Prior Authorization Description of Procedure Code Medical Records Request Information Required 19316 SUSPENSION OF BREAST Pre-operative evaluation history and physical including functional impairment and operative report.
Prior Authorizations - Provider Preauthorization for Services BCBS of WNY. Blue Shield of California Promise Health Plan. Precertification is required for many services including the following outpatient hospital benefits physician benefits and other covered services.
1 2021 TurningPoint Healthcare Solutions LLC manages authorization requests. The procedures or services on the below lists may require prior authorization or prenotification by BCBSTX Medical Management AIM Specialty Health or. The following documents pertain to procedures for which the Medicare Plus Blue Utilization Management department manages authorizations for dates of service prior to Jan.
Weve provided the following resources to help you understand Empires prior authorization process. We encourage you to verify that a Prior Authorization has been approved BEFORE you receive services or supplies that require a Prior Authorization. This is called a prior authorization.
To request prior authorization for these medications please submit the. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Blue Cross Blue Shield of Michigan Request for Preauthorization Form.
Https Bluecrossnc Com Sites Default Files Document Attachment Common Pdfs Hmo Ppo General Quantity Limitations Fax Request Form Pdf
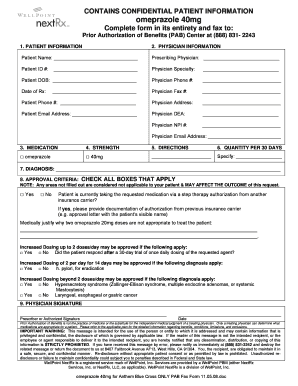 Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
Blue Cross Prior Auth Forms Pdf Fill Online Printable Fillable Blank Pdffiller
Https Www Bcbsil Com Pdf Education Forms Fhp Preauth Form Pdf
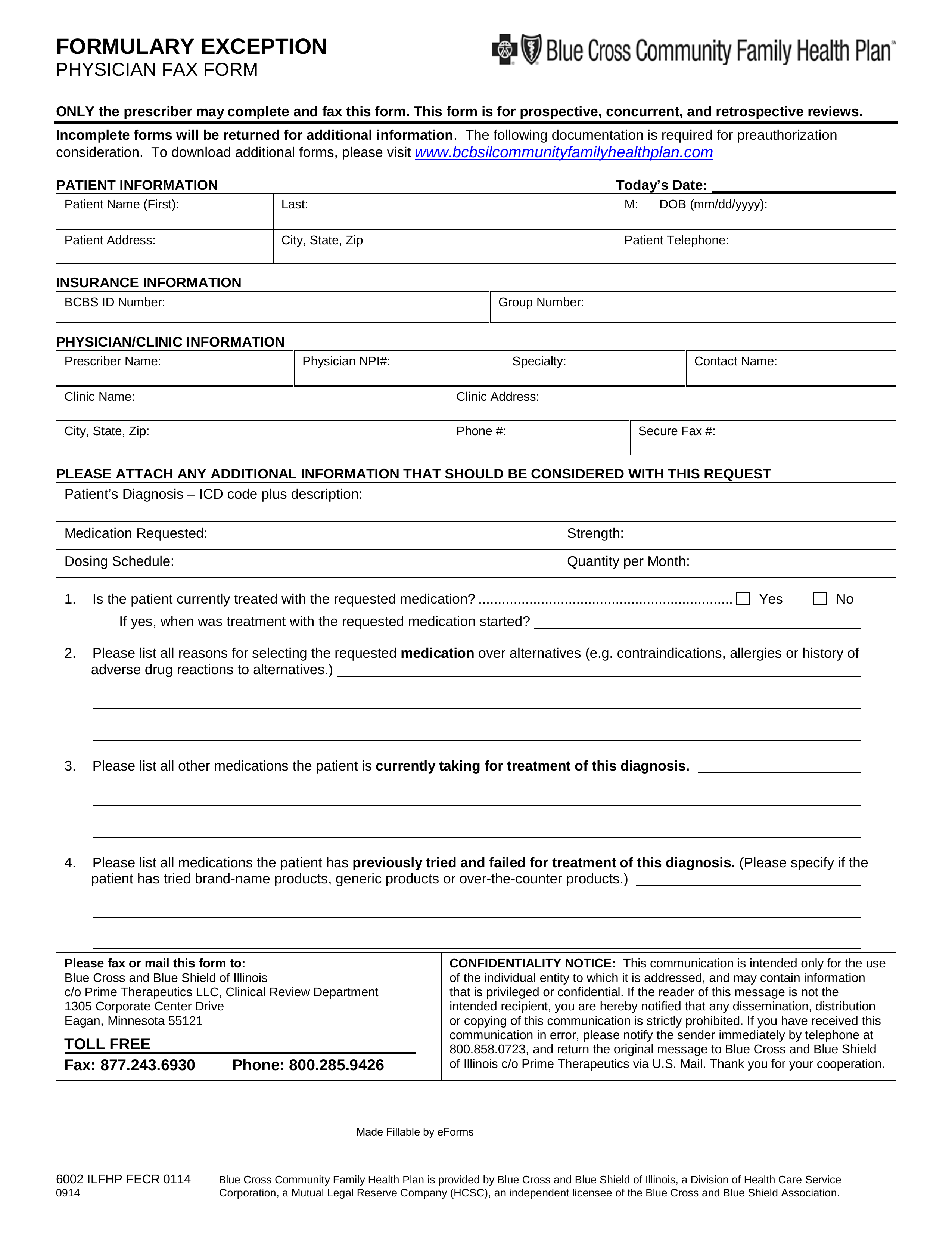 Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
Https Www Anthem Com Provider Noapplication F0 S0 T0 Pw E228625 Pdf Na Pharminfo
 2020 Texas Standard Prior Authorization Request Form For Health Care Services Fill Out And Sign Printable Pdf Template Signnow
2020 Texas Standard Prior Authorization Request Form For Health Care Services Fill Out And Sign Printable Pdf Template Signnow
 Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
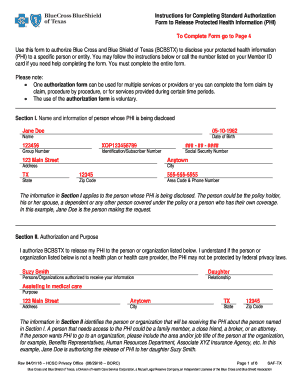
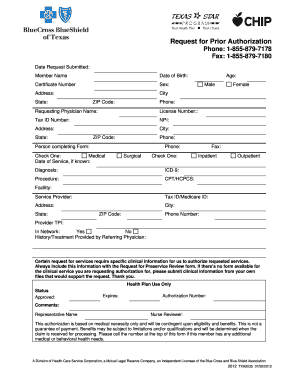 Fillable Online Bcbs Request For Prior Authorization Form Fax Email Print Pdffiller
Fillable Online Bcbs Request For Prior Authorization Form Fax Email Print Pdffiller
 Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
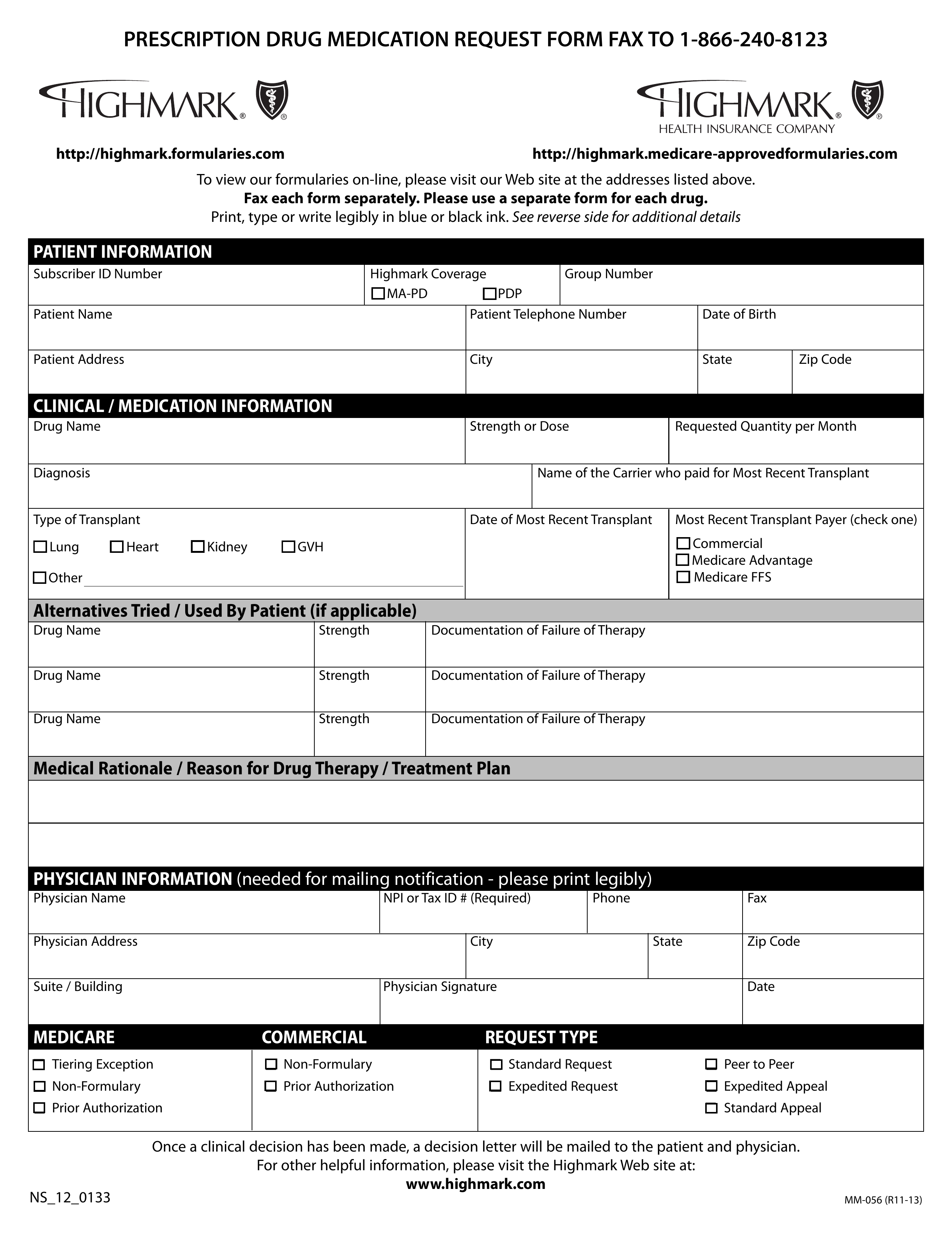
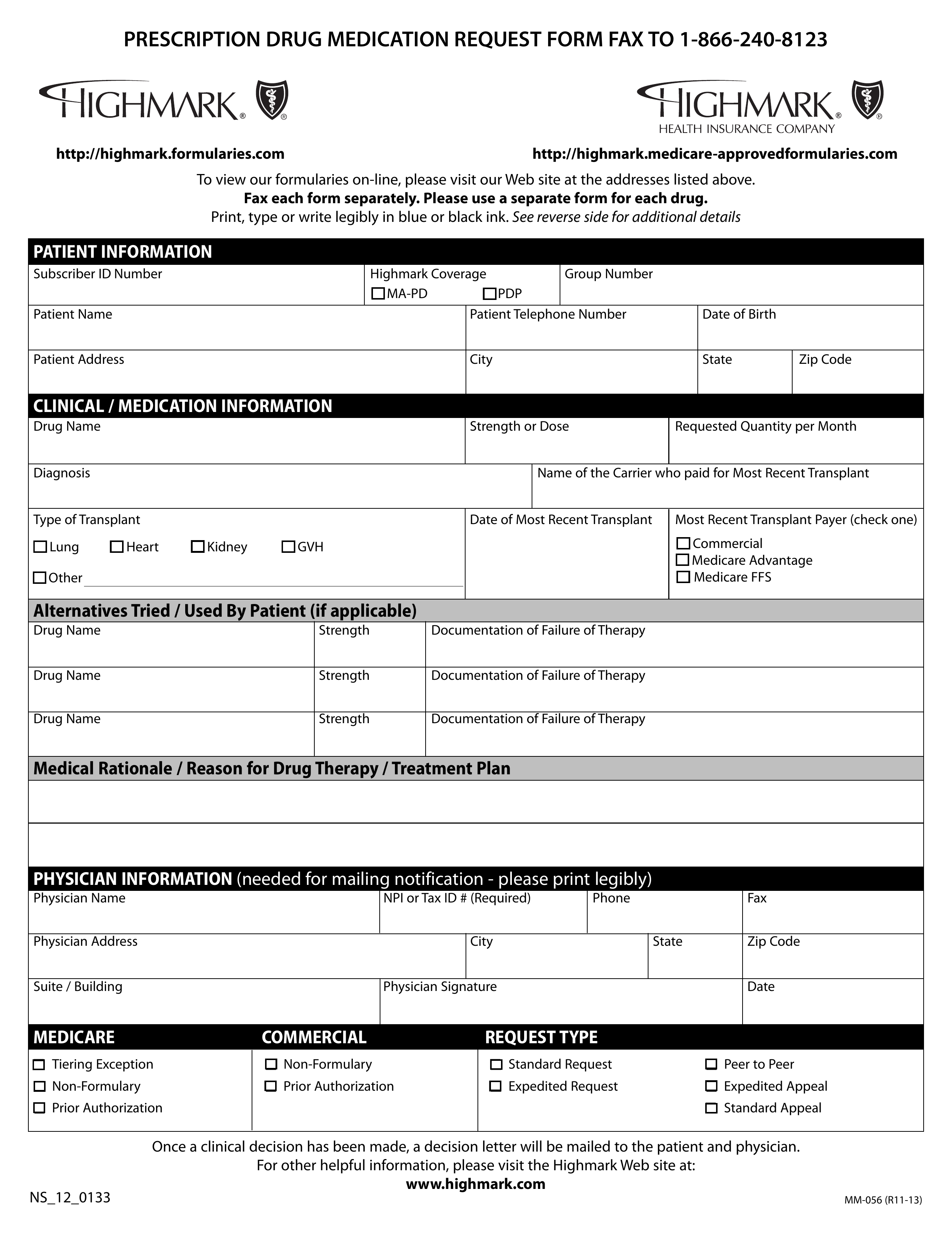 Free Highmark Prior Rx Authorization Form Pdf Eforms
Free Highmark Prior Rx Authorization Form Pdf Eforms
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
 Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Https Providers Bcbsal Org Portal Documents 10226 301829 General Prescription Drug Coverage Authorization Request Form A9b9b8bf 922b 469a B21f E396da68c634 Version 1 5
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.