Drug listFormulary inclusion does not infer a drug is a covered benefit. A non-preferred drug is a drug that is not listed on the Preferred Drug List PDL of a given insurance provider or State.
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
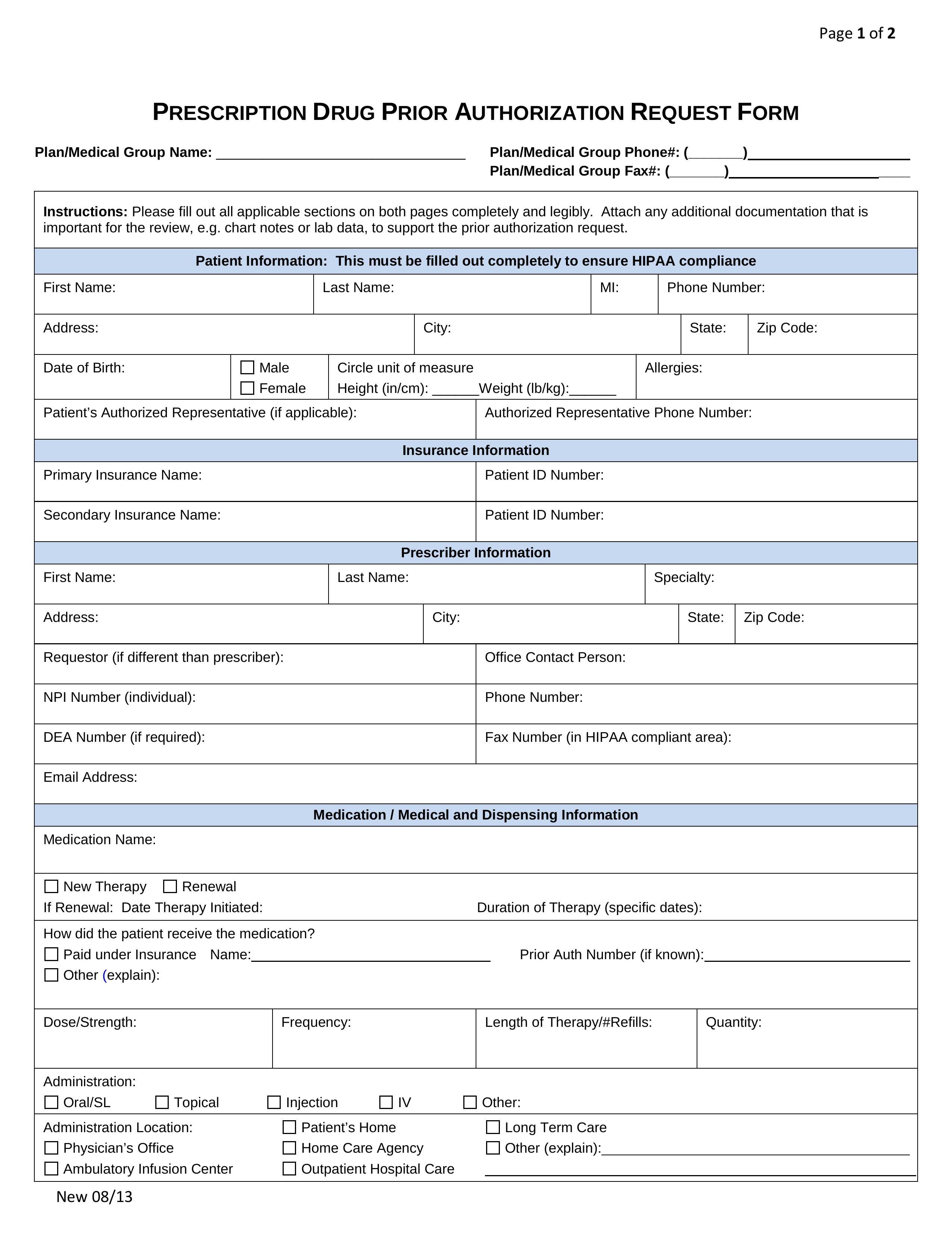
Uniform Prescription Drug Prior Authorization Form As of January 1 2019 the State of Louisiana requires all health care providers to use their state-specific form for prescription drug prior authorization requests.
Prescription prior authorization. Please check your schedule of benefits for coverage information. Health care providers should entirely fill out and submit the completed form to the fax number listed on the form. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost.
ELECTRONIC PRIOR AUTHORIZATION Electronic Prior Authorization integrates directly with EHR and pharmacy software enabling prescribers specialty pharmacists and technicians to quickly and easily obtain prior authorizations so patients can start their medications sooner. How to request precertifications and prior authorizations for patients. See our Prior Authorization List which will be posted soon or use our Prior Authorization Prescreen tool.
On the prior authorization form the person making the request must provide a medical rationale as to why the chosen. How to Get Prior Authorization after the fact. Your insurance provider.
Authorization requests may be submitted via web portal fax or phone and must include all necessary clinical information pertinent to the. Prior authorization is a requirement that your physician obtains approval from your healthcare provider before prescribing a specific medication for you or to performing a particular operation. Prescription Drug Prior Authorization Some drugs require authorization before they will be covered by the pharmacy benefit program at the point of sale.
Remember if you are approved a prior. Standard prior authorization requests should be submitted for medical necessity review as soon as the need for service is identified. Most elective services require prior authorization.
Without this prior approval your health insurance provider may not pay for your medication or operation leaving you with the bill instead. This approval process is called prior authorization. Please see the prior authorization grid for more information on the services that require prior authorization.
The physician will contact the insurance company and submit a formal authorization request. The Prior Authorization Certified Specialist PACS graduates are expanding patient access advocating for better patient outcomes and leading the reimbursement and access industry. Prescription prior authorization forms are used by physicians who wish to request insurance coverage for non-preferred prescriptions.
Your pharmacy will contact if your doctor if he or she did not obtain prior authorization from the insurance. Highmark members may have prescription drug benefits that require prior authorization for selected drugs. To request a review to authorize a patients treatment plan please complete the prior authorization request form and fax it to the Utilization Management Department at 1-408-874-1957 along with clinical.
Prior authorization is an approval required by many health insurers before they will cover certain prescriptions procedures or tests. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. Prior authorization can help lower the cost of expensive prescriptions by first requiring you to try a lower cost alternative thats equally effective.
Your insurer will then decide whether or not to cover your medicine and you should hear back from your pharmacist about their decision within two days. Enter in the following data. Depending on a patients plan you may be required to request a prior authorization or precertification for any number of prescriptions or services.
Required Clinical Information Provide all relevant clinical information to support a prior authorization Provide symptoms lab results with dates andor justification for initial or ongoing therapy or increased dose and if patient has any contraindications for the. Fidelis Prior Prescription Authorization Form Step 2 The first information required pertains to the member for whom coverage is being requested as well as the individual prescribing the drug in question. Reduces Administrative Burdens and.
The process also allows your health insurance company to review your prescriptions looking for any potentially dangerous drug interactions that your doctor may have been unaware of when prescribing. A full list of CPT codes are available on the CignaforHCP portal. Submit or Check Status of Prior Authorization for Prescriptions expand_more Check current prescription coverage and price including out-of-pocket prescription costs for UnitedHealthcare members at their selected pharmacy with the PreCheck MyScript Tool on Link.
If your prescription requires a prior authorization the pharmacy will notify your healthcare provider who will provide the necessary information to your insurance company. Some drugs and certain amounts of some drugs require an approval before they are eligible to be covered by your benefits. Establish Yourself as an Expert in Prior Authorization Increase your effectiveness while making a.
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
![]() Oh No My Prescription Requires A Prior Authorization Now What Don T Fill Your Prescription
Oh No My Prescription Requires A Prior Authorization Now What Don T Fill Your Prescription
 Free Prior Rx Authorization Forms Pdf Eforms
Free Prior Rx Authorization Forms Pdf Eforms

 Electronic Prior Authorization For Faster Approvals Surescripts
Electronic Prior Authorization For Faster Approvals Surescripts
 The Ultimate Guide To Prior Authorization Myndshft
The Ultimate Guide To Prior Authorization Myndshft
 Oh No My Prescription Requires A Prior Authorization Now What Don T Fill Your Prescription
Oh No My Prescription Requires A Prior Authorization Now What Don T Fill Your Prescription
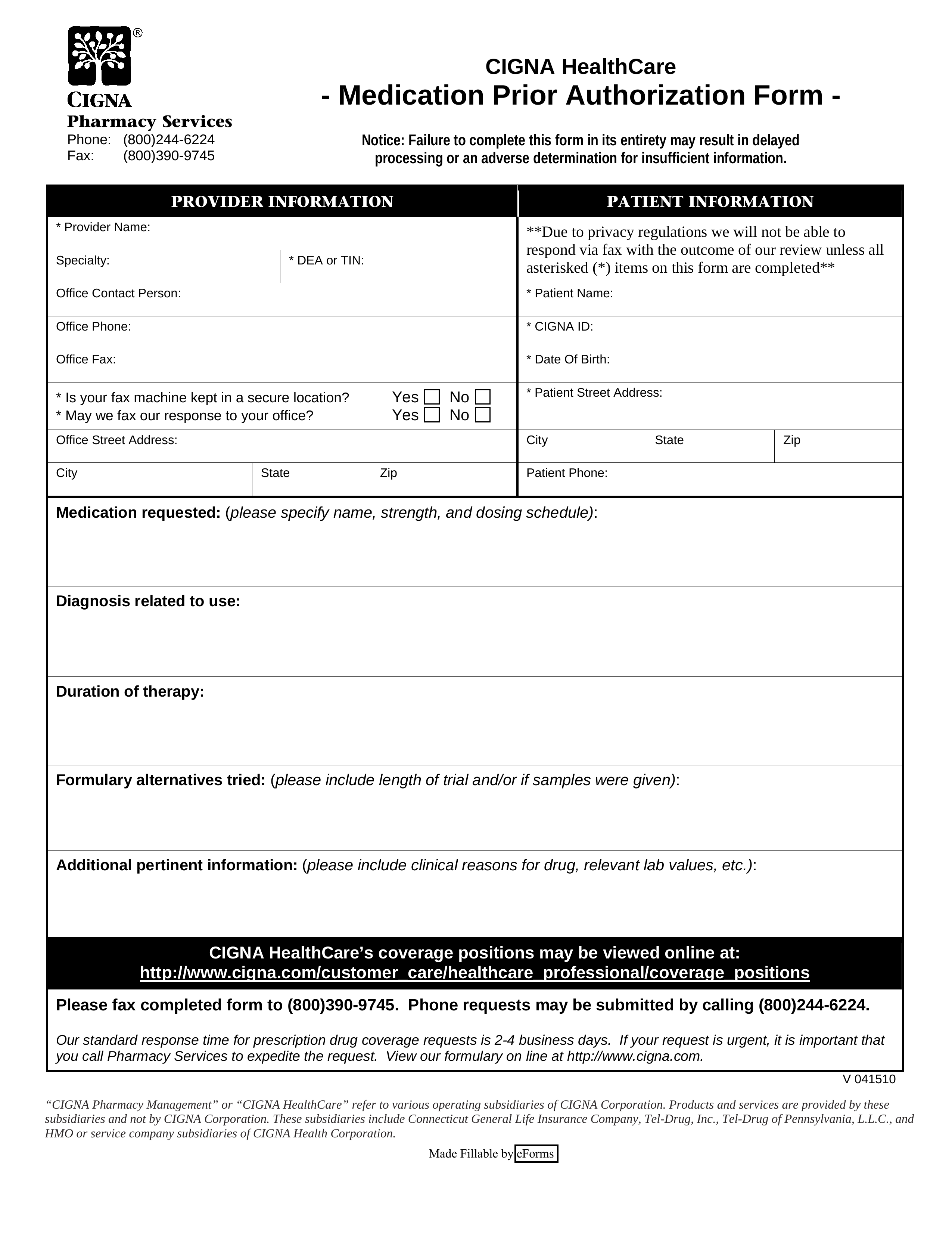 Free Cigna Prior Rx Authorization Form Pdf Eforms
Free Cigna Prior Rx Authorization Form Pdf Eforms
 Electronic Prior Authorization Practice Fusion
Electronic Prior Authorization Practice Fusion
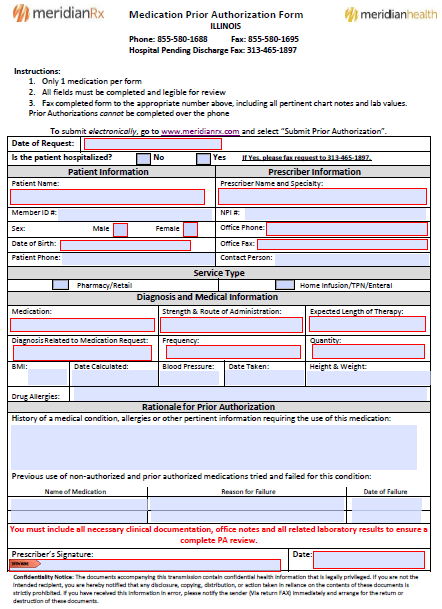 Meridian Prior Prescription Rx Authorization Form Authorization Forms
Meridian Prior Prescription Rx Authorization Form Authorization Forms
 The Ultimate Guide To Prior Authorization Myndshft
The Ultimate Guide To Prior Authorization Myndshft
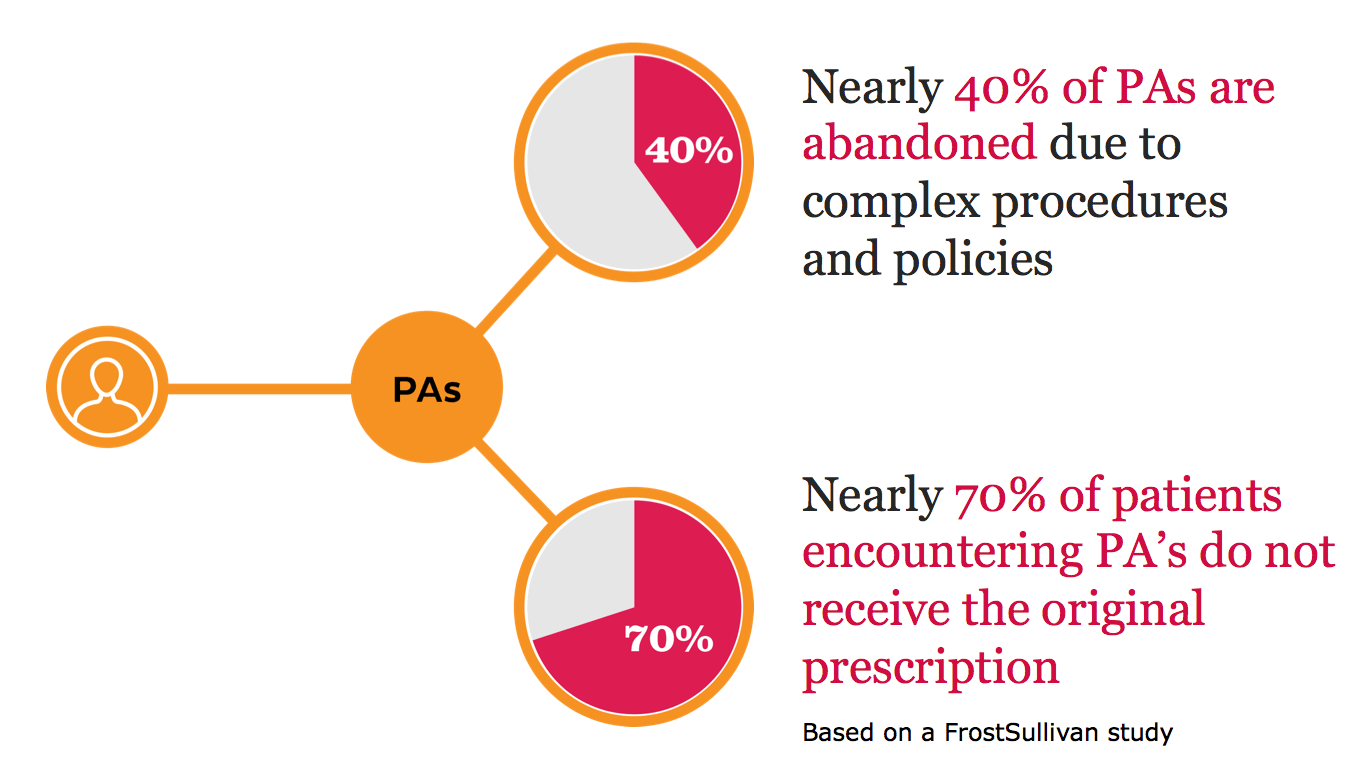
 The Shocking Truth About Prior Authorizations In Healthcare
The Shocking Truth About Prior Authorizations In Healthcare
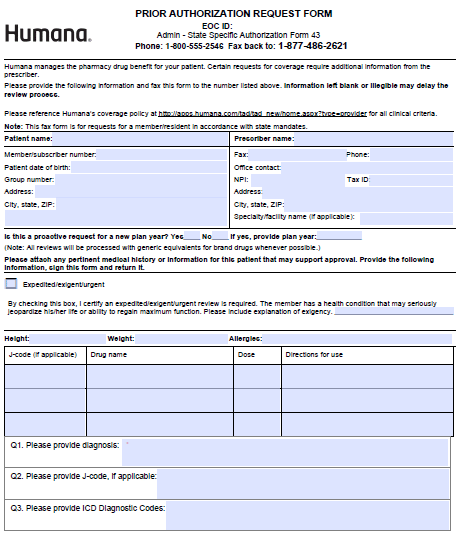 Humana Prior Prescription Rx Authorization Form Authorization Forms
Humana Prior Prescription Rx Authorization Form Authorization Forms
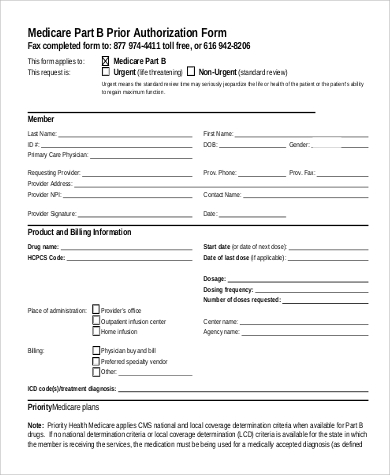 Free 9 Sample Prior Authorization Forms In Ms Word Pdf
Free 9 Sample Prior Authorization Forms In Ms Word Pdf

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.