Pharmacy benefit manager change to IngenioRx Sep 1 2019 State Federal Cal MediConnect Effective January 1 2020 IngenioRx will become our new pharmacy benefit manager PBM and will start managing prescription coverage for your Anthem Blue Cross Cal MediConnect Plan Medicare-Medicaid Plan individual and group retiree plan patients. Preferred Drug List PDL.
O Meets certain age and other specified criteria.

Anthem blue cross pharmacy coverage. Members who are speec h- or hearing-im pair ed sh ould call 1 -800-22 1-6915 TD DT TY M onday to Friday 830 a m. You can save money when your doctor prescribes medications on the drug list. Anthem also covers many over-the-counter OTC medicines with a prescription from your doctor.
If you have prescription drug coverage through Blue Cross and Blue Shield of Illinois BCBSIL this information can help you and your doctor get the most from your prescription drug coverage. Find a Participating Pharmacy. We have two drug lists that show which drugs are in your plan.
PHARMACY AND PRESCRIPTION PLAN INFORMATION. Anthem Blue Cross and Blue Shield Anthem prescription drug benefits include medications on the Anthem Preferred Drug List. To verify pharmacy network participation or Anthem Blue Cross Anthem drug coverage please call the Pharmacy Benefits manager.
You may save money by using lower tier drugs. Fill your prescription drugs You can bring your Anthem Blue Cross Cal MediConnect Plan card and your prescription to a network pharmacy or a mail-order pharmacy. To 5 pm Eastern tim e.
These guidelines impact all our products with the. Drug coverage information. Bronze HRA Coverage for.
You may need to get approval from us for certain drugs. The Anthem Preferred Drug List also called a formulary has drugs on it that are approved by the US. For example drugs used for cosmetic purposes usually are not covered.
Jul 1 2020 Guideline Updates Coverage and Clinical Guidelines. IndividualFamily Plan Type. All of our members can access a network of over 60000 Preferred pharmacies across the US.
Click here to access your pharmacy network. The Anthem Blue Cross and Blue Shield Healthcare Solutions Anthem PDL includes all medicines covered by Medicaid. O Obtains prescriptions for OTC and pharmacy items from in-network doctors or other in-network health care.
Members do NOT have to go to a CVS pharmacy location for their prescriptions. CVS Caremark will administer the pharmacy benefits for members and their Covered Dependents enrolled in Anthem Blue Cross and Blue Shield and UnitedHealthcare Non-Medicare Advantage Plan Options. You YouSpouse or Children You Family Plan TypeHRA The Summary of Benefits and Coverage SBC document will help you choose a health plan.
Your request should include why a specific drug is needed and how much is needed. Simply show your member ID card at the pharmacy. Anthem Blue Cross Cal MediConnect Plan works with many pharmacies in Santa Clara County.
Anthem covers certain over the counter OTC drugs and other pharmacy items at 100 when the member. Or visit us at. View listings below of the retail pharmacies that participate in our pharmacy networks.
Anthem Blue Cross and Blue Shield in Virginia and our affiliate HealthKeepers Inc will implement the following new and revised coverage guidelines effective October 1 2020. Coverage guidelines effective October 1 2020. There is no deductibleyou only pay your applicable cost share amounts based on the drug tier and your coverage type.
Commonly used over-the-counter OTC items are available once you receive a prescription from your provider. If you are a member with Anthems pharmacy coverage click on the link below to log in and search for network pharmacies. And we cover a wide range of brand-name and generic drugs.
What is a Drug List. Bring your Anthem Blue Cross Cal MediConnect Plan card and your prescription to a network pharmacy. Anthem Blue Cross and Blue Shield Drug List Your prescription drug benefit includes coverage for medications that youll find on the Anthem Preferred Drug List.
Be sure to review. You can also use a network mail-order pharmacy. CVS Caremark has a broad pharmacy network.
You can find these items in the List of Covered Drugs under Tier 4. Your benefits include a wide range of prescription drugs. Anthem Blue Cross CalPERS PERSCare Basic Plan.
Anthem Blue Cross and Blue Shield. This is known as prior authorization PA. 01012015 12312015 Summary of Benefits and Coverage.
If you have prescription drug coverage through Blue Cross and Blue Shield of Texas BCBSTX this information can help you and your doctor get the most from your prescription drug coverage. What this Plan Covers What it Costs. If you are a BCBSIL member log in to Blue Access for Members SM BAM SM to check your drug list and learn more about your prescription drug benefits.
The SBC shows you how you and the plan would share the cost for covered health care services. Your coverage has limitations and exclusions. Prescription drugs are a vital part of your health care coverage.
 Summary Of Health Plan Payments Myblue
Summary Of Health Plan Payments Myblue
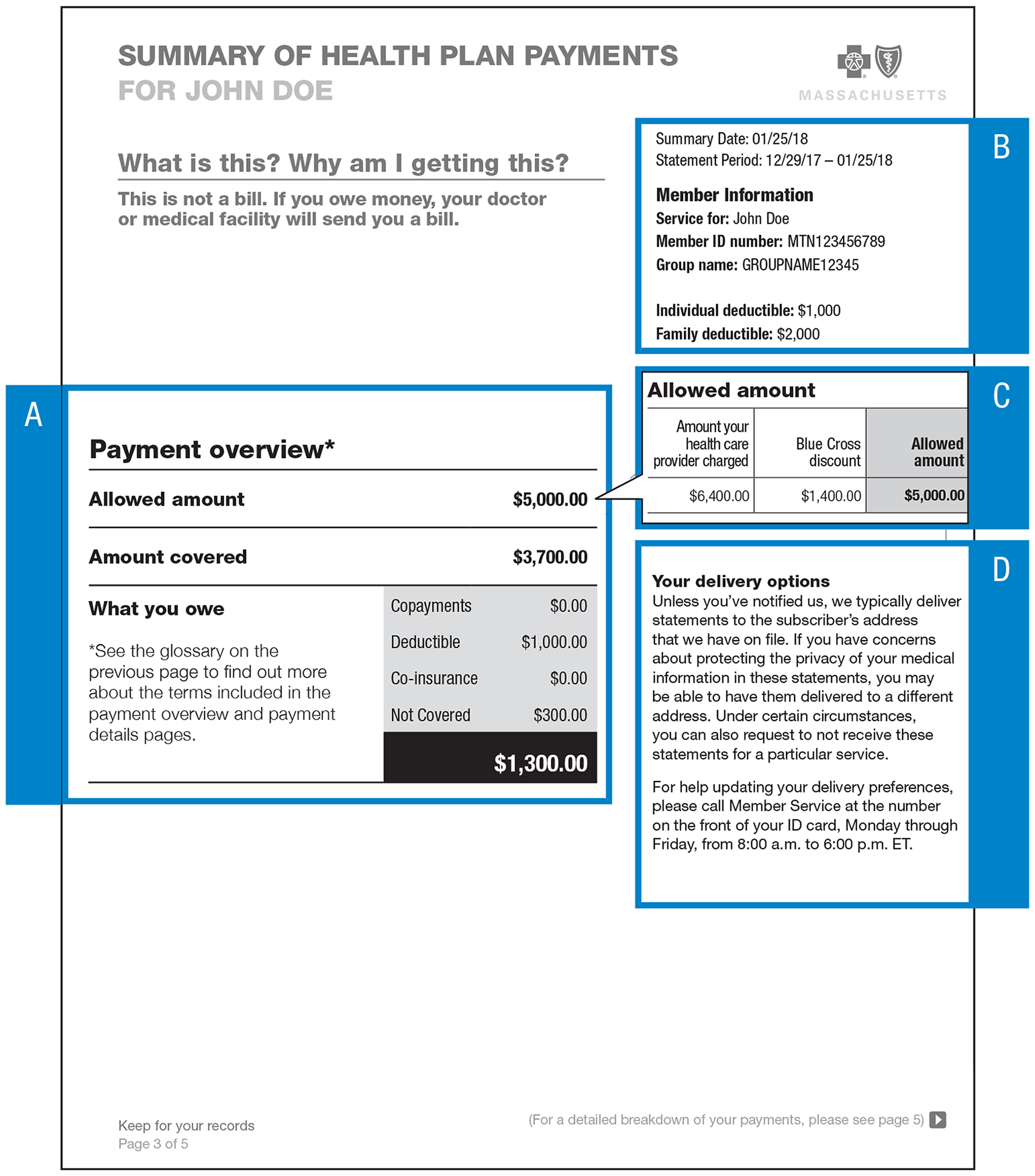 Summary Of Health Plan Payments Myblue
Summary Of Health Plan Payments Myblue
Https Www11 Anthem Com Ca Provider F0 S0 T0 Pw G320449 Pdf Refer Provider
Https Www11 Anthem Com Provider Co F5 S1 T0 Pw G298733 Pdf Refer Ahpprovider
 Individual And Employer Prescription Coverage Bcbs Of Tennessee
Individual And Employer Prescription Coverage Bcbs Of Tennessee
 Prescription Drugs Drug Search Blue Cross Blue Shield Of North Carolina
Prescription Drugs Drug Search Blue Cross Blue Shield Of North Carolina
 April 2020 Anthem Provider News And Important Updates Colorado
April 2020 Anthem Provider News And Important Updates Colorado
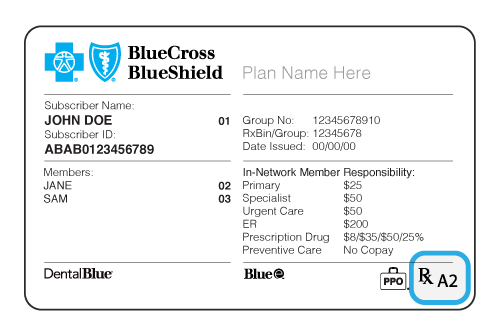
 Get Id Cards University Of California Ppo Plans
Get Id Cards University Of California Ppo Plans
Https Www Anthem Com Health Insurance Nsecurepdf Pharmacy Abcbs Anthem Natl Dl Tiered







No comments:
Post a Comment
Note: Only a member of this blog may post a comment.