This patients benefit plan requires prior authorization for certain medications in order for the drug to be covered. CVS Caremark Prior Authorization PA tools are developed to ensure safe effective and appropriate use of selected drugs.
Https Www Fchp Org Media Files Providerpdfs Forms Caremarkpaform Ashx La En
Weve partnered with CoverMyMeds and Surescripts making it easy for you to access electronic prior authorization ePA via the ePA vendor of your choice.

Cvs pharmacy prior authorization. If you would like to view forms for a specific drug visit the CVSCaremark. CVS Caremark is launching a pilot of a real-time integrated electronic prior authorization ePA capability that will be available to CVS Caremark Pharmacy Benefit Management PBM clients to help improve the patient experience and speed access to prescription medications. If you take one of these medications you and your doctor will be notified that prior.
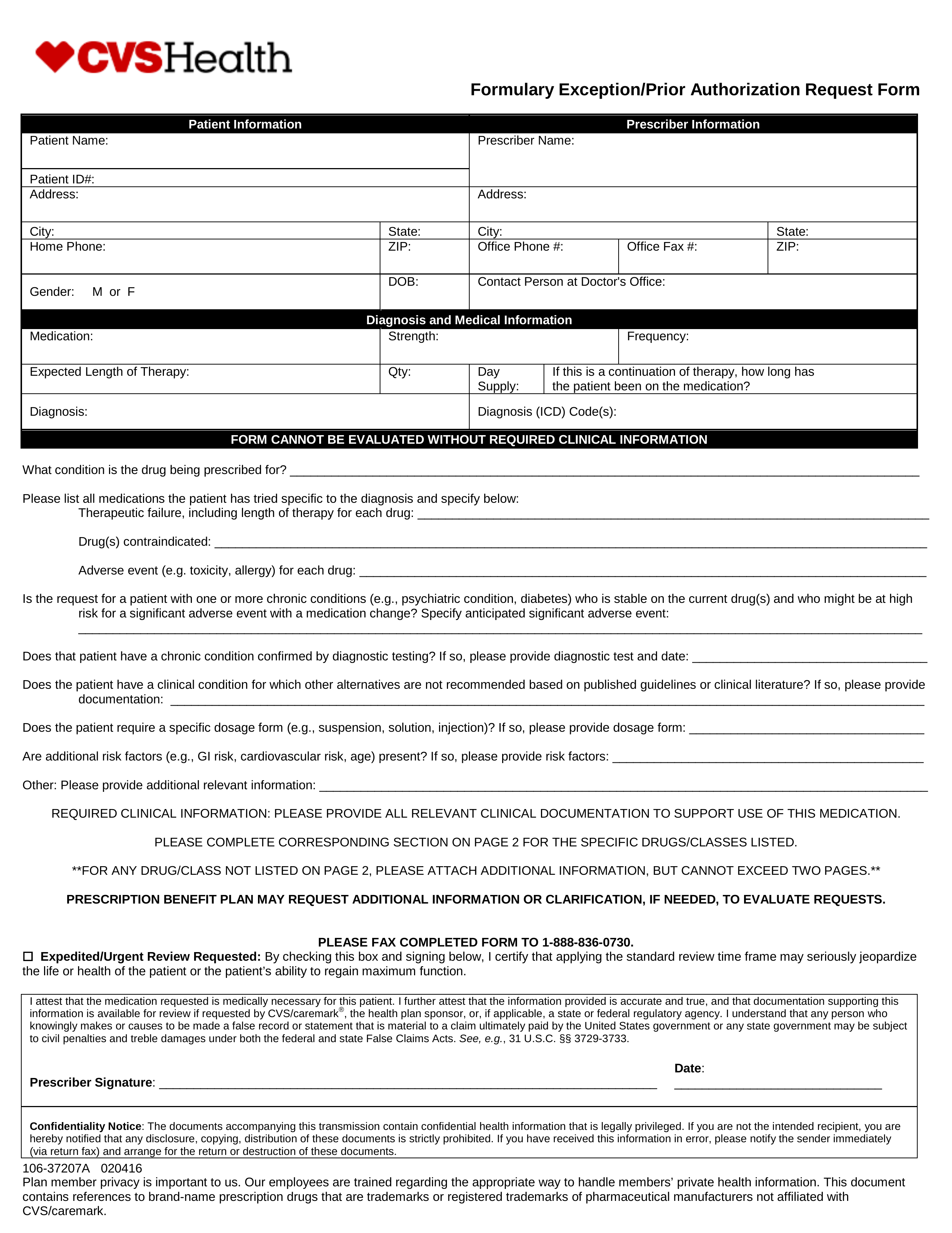
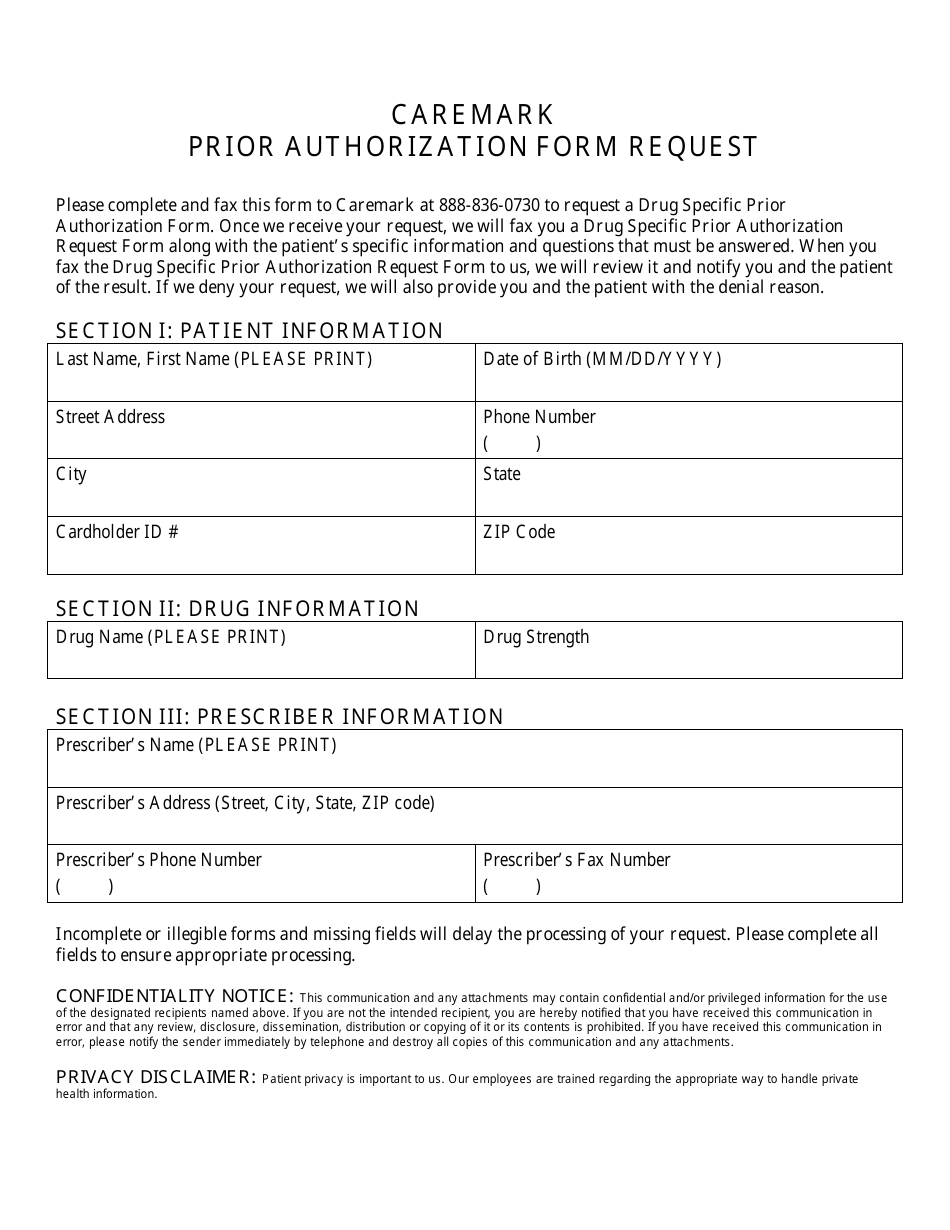
In doing so CVSCaremark will be able to decide whether or not the requested prescription is included in the patients insurance plan. Parents or guardians can sign for children. What is the prior authorization program.
Prior authorization must be approved by CVScaremark. When you join youll need to sign a Privacy Authorization. A successful pilot would represent the first step toward the.
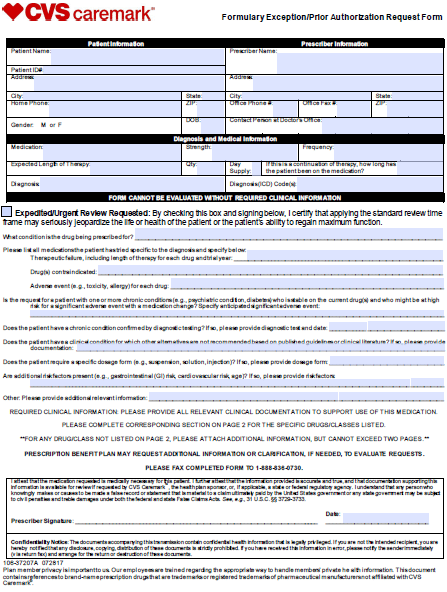
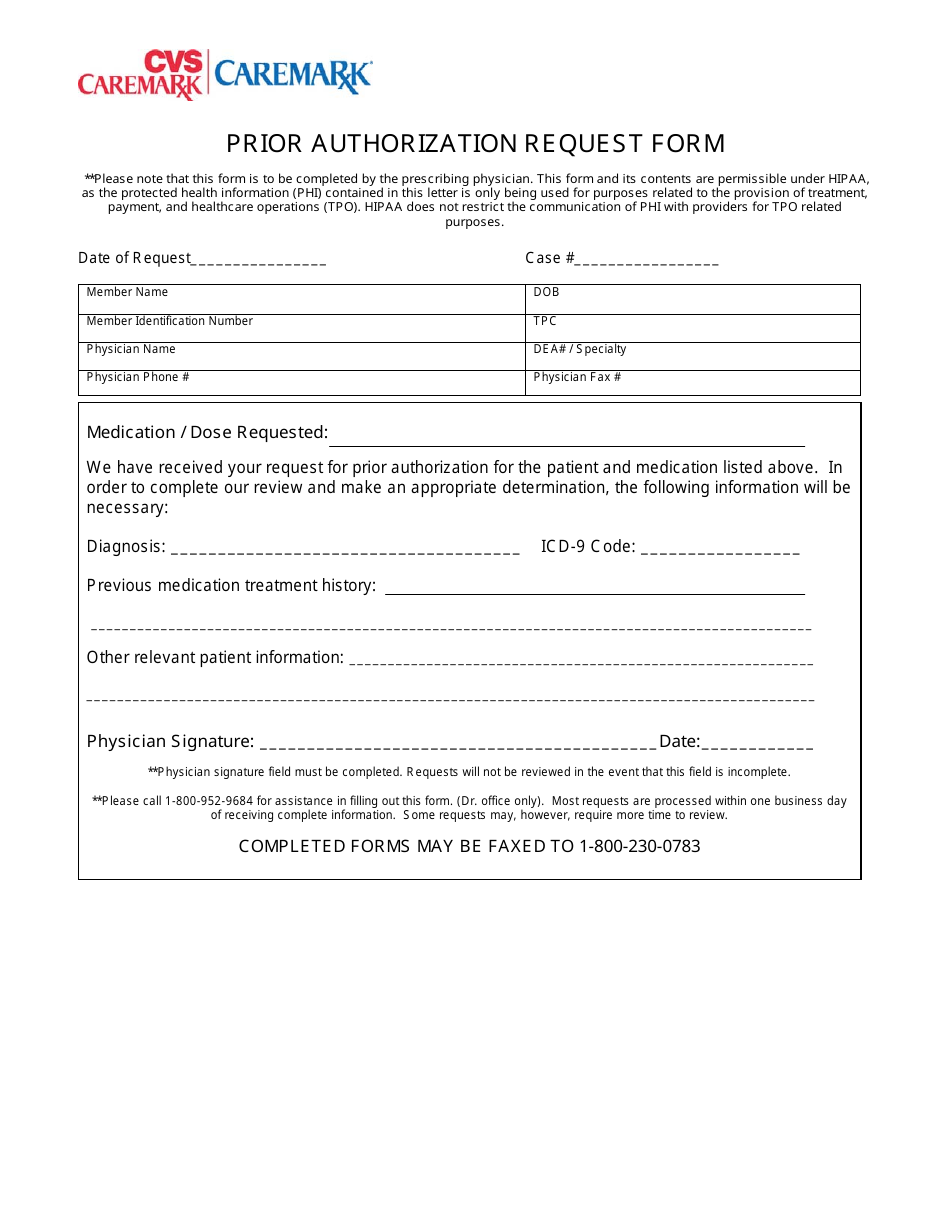
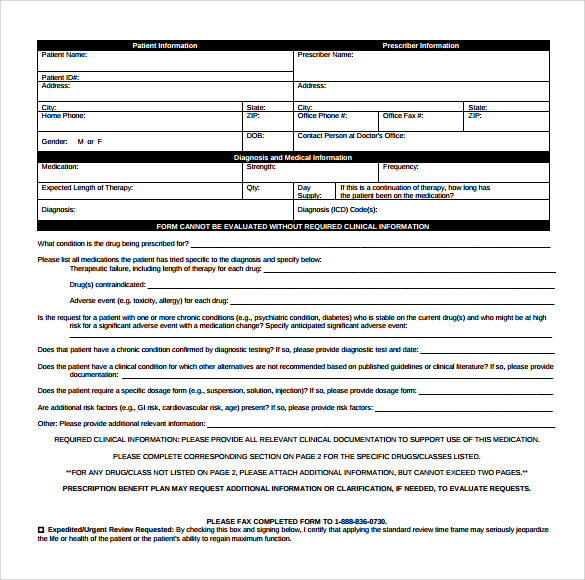
Some automated decisions may be communicated in less than 6 seconds. This authorization allows CVS Pharmacy to record the prescription earnings of each person who joins the ExtraCare Pharmacy Health Rewards program. A physician will need to fill in the form with the patients medical information and submit it to CVSCaremark for assessment.
Learn more about the Pharmacy Technician - Prior Authorization And Appeals position available at CVS Caremark. Please contact Customer Care at 866-329-4023 if you would like to confirm the price of this medication. Adults 18 years and older must sign individually.
Job Description This position will be working from home with potential to go into the Houston TX or Phoenix AZ offices once COVID restrictions are lifted. CVS Caremark has made submitting PAs easier and more convenient. Certain brand drugs that have significantly lower generic or over-the-counter alternatives available will require prior authorization before the brand drug can be filled.
Prior Authorization Specialist - Pharmacy Technician. 8-11 Per Hour Glassdoor est Show Salary Details. A separate authorization is necessary for each person who joins.
Apply to Pharmacy Technician Authorization Specialist Independent Representative and more. Prior Authorization Pharmacy Technician CVS Health Phoenix AZ 3 days ago Be among the first 25 applicants. View qualifications responsibilities compensation details and more.
CVS Health New York NY. Results may indicate prior authorization is required. Here is what your colleagues are saying about ePA.
PA Forms for Physicians. See who CVS Health has hired for. If your prescription requires a prior authorization the pharmacy will notify your healthcare provider who will provide the necessary information to your insurance company.
The CVSCaremark prior authorization form is to be used by a medical office when requesting coverage for a CVSCaremark plan members prescription. PHARMACY TECHNICIANCOMMERICAL PRIOR AUTHORIZATION Current Employee - San Antonio TX - January 22 2019 Not much to say CVS Health may be a great company but CVS Caremark overworks its employees and treats them like slaves. HMSA - Prior Authorization Request CVS Caremark administers the prescription benefit plan for the patient identified.
Prior Authorization Pharmacy Technician. Your insurer will then decide whether or not to cover your medicine and you should hear back from your pharmacist about their decision within two days. CVS Health Houston TX.
You get marked up for everything even if you take an extra minute in the bathroom. Remember if you are approved a prior authorization. The schedule is varied and will most likely start with M - F 11A-730P but.
Prior Authorization can ensure proper patient selection dosage drug administration and duration of selected drugs. To make an appropriate determination providing the most accurate diagnosis for the use of the. Prior Authorization Program Q.
Apply to Pharmacy Technician Medical Director Prior Authorization Specialist and more.
Cvs Caremark Specialty Pharmacy Prior Authorization Form Humira
 Cvs Specialty What Is A Prior Authorization
Cvs Specialty What Is A Prior Authorization
 Cvs Caremark Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Cvs Caremark Prior Authorization Form Fill Online Printable Fillable Blank Pdffiller
Https Www Osc Ct Gov Benefits Docs Formulary Exception Prior Authorization Request Form October 202017 Pdf
Http Www Ultrabenefits Com Sitecore Content Fallon Total Care Providers Pharmacy Media Ftc Pharmacyforms Ftc Caremarkpriorauthform Ashx
 Cvs Caremark Prior Authorization Form 600x800 Free Job Application Form
Cvs Caremark Prior Authorization Form 600x800 Free Job Application Form
 Cvs Prior Prescription Rx Authorization Form Authorization Forms
Cvs Prior Prescription Rx Authorization Form Authorization Forms
 Prior Authorization Request Form Cvs Caremark Download Printable Pdf Templateroller
Prior Authorization Request Form Cvs Caremark Download Printable Pdf Templateroller
 Cvs Caremark Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Cvs Caremark Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
 Streamlined Prior Authorization At The Point Of Prescribing
Streamlined Prior Authorization At The Point Of Prescribing
 Free 8 Sample Caremark Prior Authorization Forms In Pdf
Free 8 Sample Caremark Prior Authorization Forms In Pdf
 Cvs Caremark Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
Cvs Caremark Prior Authorization Form Fill Out And Sign Printable Pdf Template Signnow
 Free Cvs Caremark Prior Rx Authorization Form Pdf Eforms
Free Cvs Caremark Prior Rx Authorization Form Pdf Eforms
 Prior Authorization Form Request Cvs Caremark Download Printable Pdf Templateroller
Prior Authorization Form Request Cvs Caremark Download Printable Pdf Templateroller

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.