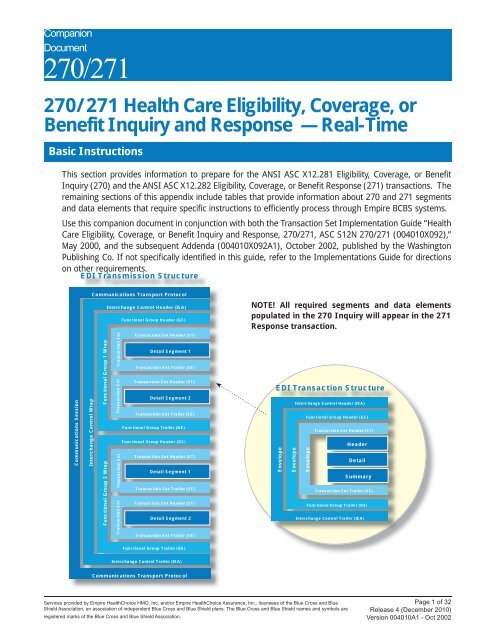
270271 Health Care Eligibility Benefit Inquiry and Response HIPAA Guidelines for Electronic Transactions Companion Document for Mandatory Reporting Non-GHP Entities For the 271 we use multiple eligibility response in one transaction set STSE and one functional group GSGE and one interchange ISAIEA per file. Version 54 1.
Https Www Cms Gov Research Statistics Data And Systems Cms Information Technology Hetshelp Downloads Hets270271companionguide5010 Pdf
The EDI 271 Health Care EligibilityBenefit Response transaction set is used to provide information about healthcare policy coverages relative to a specific subscriber or the subscribers dependent seeking medical services.
Edi 270 271. This transaction is typically sent by insurance companies government agencies like Medicare or Medicaid or other organizations that. After careful review of the existing IG for the Version 005010X279A1 we have compiled the UnitedHealthcare specific CG. Complete the form as appropriate using the information provided below.
ASC X12N 270271 005010X279A1 Independence Administrators is an independent licensee of the Blue Cross and Blue Shield Association. For understanding how it can help you and how to get started check out the dropdowns below. Certification Statement for Provider Billing Medicaid.
The Health Insurance Portability and Accountability Act HIPAA requires health insurers nationwide comply with Electronic Data Interchange EDI standards for health care established. ETIN 0SN zero S N Billing Service Name If Applicable. EDI enrollment processing timeframe is approximately 10 business days.
Via a standard 270271 EDI transaction to the BSC EDI system. Please note that this is UnitedHealthcares approach to the 270271 eligibilit y and benefits transactions. EDI adoption has been proved to reduce the administrative burden on providers.
The 270 transaction is used to request eligibility and benefit information for Medical and Behavioral lines of business and the 271 transaction is used to respond with this information for the specified member. 270271 transaction set in the electronic data interchange EDI environment. 270 271 Healthcare transactions their relationship functions and purposes will be described further in the post.
270271 Overview The 270 is used by a provider to request eligibility coverage and benefit information from a payer The 271 is used by the payer to respond to a providers request for eligibility coverage and benefit information. It is sent in response to a 270 inquiry transaction. Member ID Provider ID The other fields on the Eligibility Request screen will be the Eligibility Start Date and Provider ID fields.
To check status of EDI enrollment please contact Medicaid at 800-343-9000. The 271 is the Health Care EligibilityBenefit Response and is used to transmit the information requested in a 270. 270 271 Healthcare Eligibility Coverage and Benefit Inquiry 270 and Response 271 EDI Transaction Definition.
Aetna SSI 270271 Companion Guide 9 TRANSMISSION ADMINISTRATIVE PROCEDURES Aetna SSI will return a 271 response or 999 in case of failed validation within 20 seconds of receiving the 270 request from Emdeon to provide as close to a real-time response as possible. The ISDH posts the responses within a reasonable amount of time for the requestor to retrieve. The 270 transaction is used to request eligibility and benefit information for medical lines of business and the 271 transaction is used to respond with information.
Format and data content of the Eligibility and Benefit 270271 transaction set in the Electronic Data Interchange EDI environment. Eligibility Benefit Inquiry and Response 270271 Eligibility Status Request 270 The only data elements that are required by Health Partners to identify the member are. It is set to receive care from a Provider.
BSC EDI is a system through which trading partners can submit 270 EDI transactions as well as receive 271 EDI transactions. The Eligibility and Benefit Response 271 transaction is used to respond to a 270 inquiry about the health care eligibility and benefits associated with a subscriber or dependent. A batch request or inquiry transaction 270 results in the creation of the response transaction 271.
Section 2 provides communication specifications for data exchange. This document describes how a submitter uses the system to. 270271 Companion Guide for NGHP Entities Introduction and Purpose.
The EDI 271 Healthcare EligibilityBenefit Response transaction set is used to provide information about healthcare policy coverages relative to a specific subscriber or the subscribers dependent seeking medical services. The 270 transaction is the EDI function that requests eligibility and benefit information from the Insurance Company of the patient. The 270 transaction is used in conjunction with the EDI 271 transaction.
It is sent in response to a 270 inquiry transaction.
Https Www Tricare West Com Content Dam Hnfs Tw Prov Resources Pdf Claims 270 271 Guide Pdf
 270 271 Health Care Eligibility Coverage Or Benefit Inquiry And
270 271 Health Care Eligibility Coverage Or Benefit Inquiry And
Https Www Fideliscare Org Portals 0 Providers Guides 2019 Fideliscare Companionguide 270271 English Pdf
270 271 Edi Transactions Relationshipedi Blog Edi Blog
Cigna 270 And 271 Eligibility And Benefitsedi Blog Edi Blog
Https Www Medicaid Nv Gov Downloads Provider Health Care Elig Benefit Inquiry Information Response 270 271 Pdf
 Edi 270 Power Generator Ems Healthcare Informatics Ems Healthcare Informatics
Edi 270 Power Generator Ems Healthcare Informatics Ems Healthcare Informatics
Http Www Ehcca Com Presentations Ehc Info3 Beatty2 Pdf
Https Www Cms Gov Research Statistics Data And Systems Cms Information Technology Hetshelp Downloads Hets270271companionguide5010 Pdf
Http Www Ehcca Com Presentations Ehc Info3 Beatty2 Pdf
Https Www Ctdssmap Com Ctportal Portals 0 Staticcontent Publications Ct Aca 270 271 Companion Guide V1 0 Pdf
Https Www Uhcprovider Com Content Dam Provider Docs Public Resources Edi Edi 270 271 Companion Guide 005010x279a1 Pdf
Https Www Aetnaseniorproducts Com Ssi Assets Pdf Aetna 20ssi 20edi 20270 271 20companion 20guide Pdf
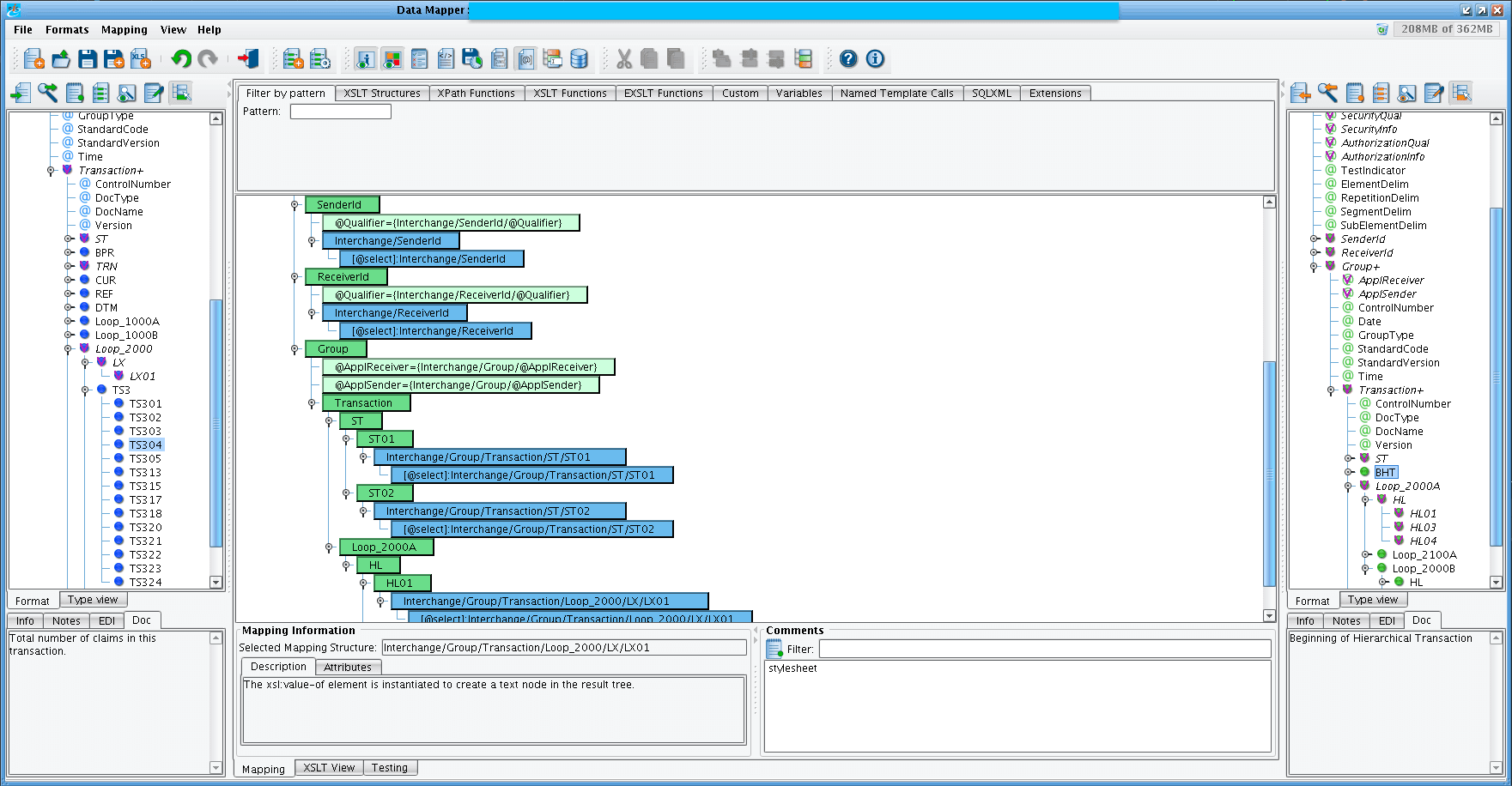 Edi 271 A1 Transaction Example Formatted With Pilotfish Data Mapper
Edi 271 A1 Transaction Example Formatted With Pilotfish Data Mapper

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.