If you engage in high-risk sexual behaviors you may want to consider being tested once a year for gonorrhea even though you don. If you have an HPV kit you may be billed 60-80 as an expected allowable.
 University Of Michigan Student Tuition Will No Longer Cover Testing For Sexually Transmitted Infections At University Health Services The Michigan Daily
University Of Michigan Student Tuition Will No Longer Cover Testing For Sexually Transmitted Infections At University Health Services The Michigan Daily
Section 2713 of the Public Health Service PHS Act as added by the Affordable Care Act and incorporated into ERISA The Employee Retirement Income Security Act of 1974 and the Code requires that non-grandfathered external icon group health plans and health insurance issuers offering non-grandfathered group or individual health insurance coverage provide coverage.

Sti testing covered by insurance. Reported by Medicaid and commercial insurance plans2 Lower than desired screening rates for STIs may be the result of several factors including stigma. Medicare Advantage Part C plans may also cover STD testing if your doctor deems it to be medically necessary. Some STIs dont cause symptoms or they can cause symptoms that go away.
With health insurance each test kit costs 75 plus the 15 consultation fee and any applicable copays or deductibles. It is important to note that if you have an STI or PrEP test kit and have not yet met your deductible you may be billed for the expected allowable for your insurance plan which is usually around 200-300. The consultation fee provides patients with unlimited access to the Nurx medical team regarding their STI results.
The USPSTF recommends testing all sexually active women ages 24 and younger. An STI test usually needs to be paid from your deductible for healthcare costs in Dutch. Some expert opinions may vary and your doctor may recommend testing based on your personal history.
Theres OraQuick the only FDA-approved at-home STI test which costs around 45 and can be purchased online or at a number of drugstore. But plans that arent considered minimum essential coverage arent required to cover COVID-19 testing. It tests for HIV chlamydia gonorrhea syphilis and hepatitis C.
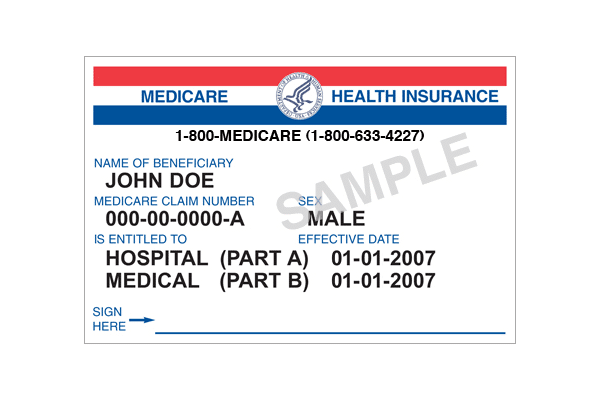
Medicare Part B Medical Insurance covers sexually transmitted infection STI screenings for chlamydia gonorrhea syphilis andor Hepatitis B if youre. The visit to your GP is free covered by your basic health insurance. Experts say that certain groups should be routinely tested for certain STIs.
Medicare Part B may cover STD testing and STI screening if youre considered high risk and the test is ordered by a doctor. STD testing can also be free or low cost with. Healthy Woman costs 190 and Full Control costs 220.
Yes most of the time. Testing for certain STDs like HIV syphilis chlamydia and gonorrhea is one of the preventive health benefits that most plans must cover under the ACA. Does health insurance cover STD testing.
Some STI tests are recommended for pregnant women whether or not they have a high risk for infection. Medicare covers STI tests for the LGBTQIA community. So unless you have a test you may not know that you have an STI.
Preventive Services Task Force USPSTF recommends a chlamydia test for all high-risk nonpregnant and pregnant women. Without health insurance Basics Covered costs 150. Some Medicare Advantage plans also cover additional preventive care services that may not be covered by Original Medicare Part A and.
At the STI clinic Some people are at greater risk of contracting an STI. As mentioned Medicare will cover STI testing for a male who has had sex with. Learn more about how to get birth control and STI testing if youre on your parents insurance plan.
Under the Families First Coronavirus Response Act Medicare Medicaid and private health insurance plans are required to fully cover the cost of COVID-19 testing. For HIV-specific concerns insurance-less options are many. These tests are usually covered by insurance and Nurx will bill your plan directly or.
Because of the Affordable Care Act aka Obamacare many insurance plans cover STD testing. So you can probably get STD testing for free or at a reduced price if you have health insurance. The USPSTF also recommends testing for women older than 24 who engage in high-risk sexual behaviors.
Once your deductible has been met only standard copays will apply.
:max_bytes(150000):strip_icc()/cigna-logo-wallpaper-e1474921230453-3d574f4097384c6eb992551dcd65822c.jpg)