The CVSCaremark prior authorization form is to be used by a medical office when requesting coverage for a CVSCaremark plan members prescription. Please complete all pages to avoid a delay in our decision.
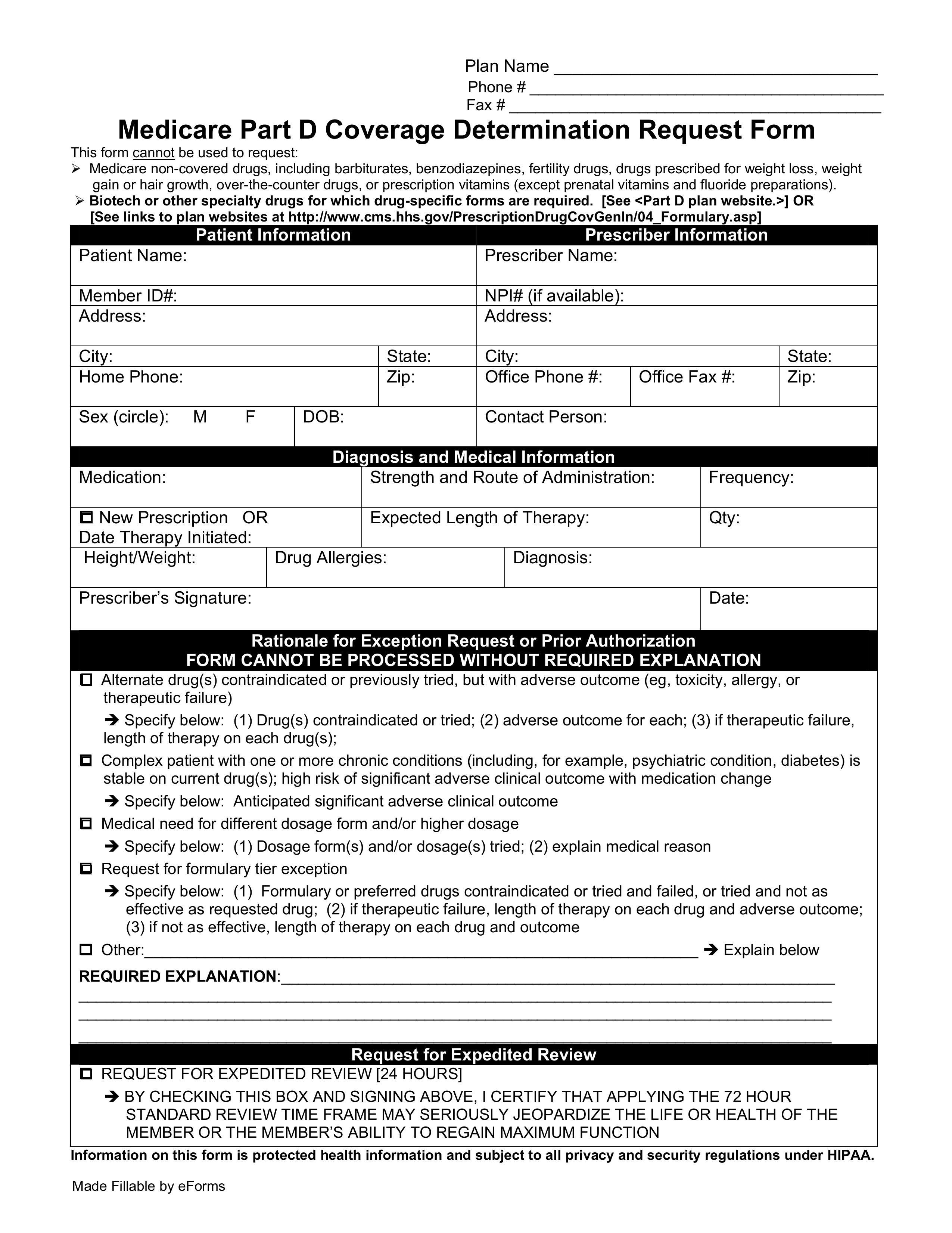 Free Medicare Prior Rx Authorization Form Pdf Eforms
Free Medicare Prior Rx Authorization Form Pdf Eforms
Prior authorization requests are defined as requests for pre-approval from an insurer for specified medications or quantities of medications before they are dispensed.
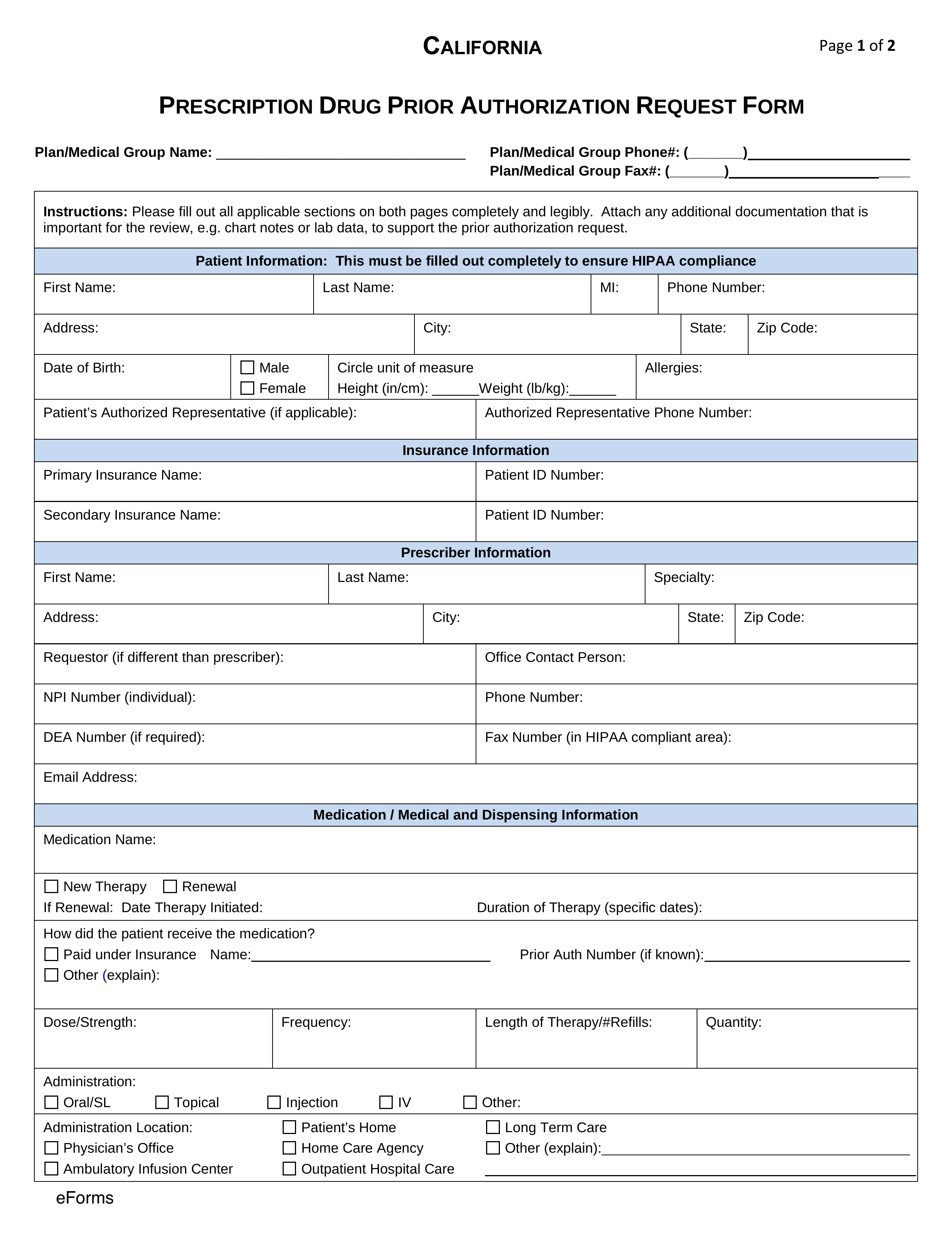
Prior authorization form for medication. Prior authorization is required for certain covered services to document the medical necessity for those services before services are rendered. Instructions are on the form. A non-preferred drug is a drug that is not listed on the Preferred Drug List PDL of a given insurance provider or State.
To ensure that prior authorizations are reviewed promptly submit request with current clinical notes and relevant lab work. Preadmission Screening and Resident Review PASRR The Preadmission Screening and Resident Review process is a requirement in all IHCP-certified nursing facilities prior to admission or when there is a significant change in the physical or mental condition of. A physician will need to fill in the form with the patients medical information and submit it to CVSCaremark for assessment.
This form may contain multiple pages. If you have questions please call 800-310-6826. KanCare Medicaid Behavioral Health PRTF Prior Authorization Request Form.
Actemra diagnosis of Giant Cell Arteritis Actemra IV Medical Actemra IV for diagnosis of Cytokine Release Syndrome CRS Medical Actemra SQ Pharmacy Non-Preferred Acthar Gel Infantile Spasms. How to Get Prior Authorization. Your authorization approval will apply to network pharmacies and home delivery.
The Medicaid prior authorization forms appeal to the specific State to see if a drug is approved under their coverage. Who reside in the state of Colorado andor. The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan.
Prescriber means the term as defined in section 17708 of the Public Health Code 1978 PA 368 MCL 33317708. If the patient has tried any preferred medications. The physician will contact the insurance company and submit a formal authorization request.
Use the Online Prior Authorization and Notification tool KanCare Medicaid Behavioral Health Inpatient Prior Authorization Request Form. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. Your insurer will then decide whether or not to cover your medicine and you should hear back from your pharmacist about their decision within two days.
Anthem has also made available a series of forms for specific medications. Acthar Gel Nephrotic Syndrome. How to Get Prior Authorization after the fact.
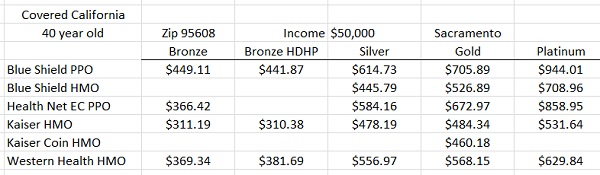
Pharmacy Prior Authorization Forms Preferred Drug List Health Resources. You dont need to send multiple forms. This form is made available for use by prescribers to initiate a prior authorization request with the health insurer.
Filled out by a physician or pharmacist this form must provide clinical reasoning to justify this request being made in lieu of prescribing a drug from the Preferred Drug List PDL. Cant Find a Form. If your prescription requires a prior authorization the pharmacy will notify your healthcare provider who will provide the necessary information to your insurance company.
Policies may vary between each states department of health but the process more or less remains the same. BHRF Admission Notification Form. Your pharmacy will contact if your doctor if he or she did not obtain prior authorization from the insurance.
Massachusetts Commercial Prior Authorization Form - Cardiac Imaging Prior Authorization Form. Member Information Prescriber Information Member Name. This form is to be completed by the patients medical office to see if he or she qualifies under their specific diagnosis and why the drug should be used over another type of medication.
PA request status can be viewed online. Download and print the form for your drug. Allow at least 24 hours for review.
Prescription drug prior authorization request form PDF opens new window. Prescription prior authorization forms are used by physicians who wish to request insurance coverage for non-preferred prescriptions. Sending an electronic Prior Authorization Form.
The PDF attached to this page is an example of a typical prescription drug. The Prior Authorization PA unit at AHCCCS authorizes specific services prior to delivery of medical related services. Prior Authorizations Forms.
The use of this form is mandated for prior authorization requests concerning commercial fully insured members. Whose prescription drug coverage was sold in the state of Colorado. Search for your drug on the TRICARE Formulary Search Tool.
Faxing 952-992-3556 or 952-992-3554. Prior Authorization Request Form Please complete this entire form and fax it to. On the prior authorization form the person making the request must provide a medical rationale as to why the chosen medication is necessary for the patient in question.
Please include ALL pertinent clinical information with your Medical or Pharmacy Prior Authorization request submission. For more information on prior authorization or to make a prior authorization. In the State of Pennsylvania Medicaid coverage for non-preferred drugs is obtained by submitting a Pennsylvania Medicaid prior authorization form.
To begin the prior authorization process providers may submit prior authorization requests to Medica Care Management by. Give the form to your provider to complete and send back to Express Scripts. Forms used in PA Unit include the following.