Hire a medical billing specialist as an advocate. How do I cancel my COBRA coverage.
 How To Sign Up For Cobra Insurance 8 Steps With Pictures
How To Sign Up For Cobra Insurance 8 Steps With Pictures
You can be required however to make an initial premium payment within 45 days after the date of your COBRA election that is the date you mail in your election form if you use first-class mail.

How to cancel my cobra insurance. I had to draft a letter and mail it to the address on my COBRA bill along with some enclosures. Since I had health coverage through my new employer as of May 1 2015 I. Termination letters can be mailed to.
I had to draft a letter and mail it to the address on my COBRA bill along with some enclosures. Generally you submit your request in writing stating you wish to cancel coverage starting on a particular date. I always thought that I could cancel a portion of my COBRA without a life event.
You should then receive a certificate of credible coverage for the time you were using COBRA. Coverage will be automatically cancelled if your payment is not postmarked on or before the deadline date of the month your premium is due. As I said my nightmare had a happy ending.
You will need to include your account number and contact information. If you have elected COBRA coverage and wish to cancel you can mail fax or email a letter to PEBP requesting termination of your coverage. Read the fine and foreboding print.
When you sign up for COBRA insurance always make a note of any special requirements your policy may have for cancellation as many times you will have to notify your previous employer in writing. Contact your former employer or its plan administrator for more details. Your benefits finally kick-in and you no longer need COBRA.
After that a notice is sent to the employee requesting acceptance or denial of the insurance continuation. Heres a copy of what I sent in case it is useful to other people. To Whom It May Concern I am writing in regard to COBRA benefits for account xxx.
Ask the employers benefits administrator or group health plan about your COBRA rights if you find out your coverage has ended and you dont get a notice or if you get divorced. You may want to keep a copy of your form for your files. You must submit your request in writing stating you wish to cancel coverage starting on a particular date.
You can lose COBRA if you move for example or if your former employer goes bankrupt. You may pay your COBRA insurance directly to the employers insurance company or you may pay it to a COBRA administrative company. Do your homework.
Send your Retiree Election form form A to the PEBB Program. Since I had health coverage through my. However if you choose to cancel coverage it cannot be reinstated.
Stop paying the premium for your COBRA. The notification you receive will give you instructions on where to send payment. Heres a copy of what I sent in case it is useful to other people.
The form must be received by the PEBB Program no later than 60 days after your employer-paid coverage COBRA coverage or continuation coverage ends. Be sure to specify the date your new group coverage begins and COBRA coverage ends. Be sure you continue to make insurance payments as long as you need the insurance.
To Whom It May Concern I am writing in regard to COBRA benefits for account xxx. You can send a letter to HealthEquity requesting termination of your COBRA coverage or you can simply stop paying premiums and your COBRA coverage will be terminated for non-payment. You will need to notify your previous employer or the plan administrator in writing that you wish to cancel.
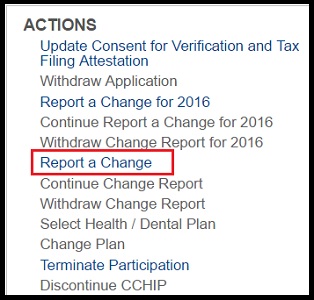
I want to cancel just my dental while maintaining me I want to cancel just my dental while maintaining me 877-262-7241 Register Now. How do I cancel my COBRA coverage. My COBRA cancellation letter.
When you elect continuation coverage you cannot be required to send any payment with your election form. My COBRA Cancellation Letter. If you are using COBRA health insurance and no longer need it you can cancel it.
If your plan does not have reasonable procedures for how to give notice of a qualifying event you can give notice by contacting the person or unit that handles. COBRA is month-to-month coverage and can be terminated at any time. COBRA general notice of the responsibility to notify the plan and procedures for doing so.
You will need to notify the plan sponsor or designated COBRA administrator to terminate your COBRA coverage. The employer must tell the plan administrator if you qualify for COBRA because the covered employee died lost their job or became entitled to Medicare. After your insurance has been canceled or terminated the employer should send you a letter notifying you of your cancellation or termination of your COBRA.
If you stop paying your coverage can be canceled. You will receive a letter from the plan administrator andor your previous employer verifying the termination of your COBRA benefits. Normally eligible employees have 60 days to accept coverage.
Once the plan administrator is notified the plan must let you know you have the right to choose COBRA. Any overpayment of premiums is returned to you. You may cancel your COBRA coverage when you obtain other insurance.
First an employer needs to speak with the health insurance provider to inform them that an employee is eligible for COBRA.