The Wellmark Authorization table is a resource to help you determine when to request a pre-service review. Prior Authorizations Lists for Blue Cross Medicare Advantage PPO SM and Blue Cross Medicare Advantage HMO SM The procedures or services on the below lists may require prior authorization or prenotification by BCBSTX Medical Management eviCore Healthcare or Magellan Healthcare.
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Get a Free Quote.
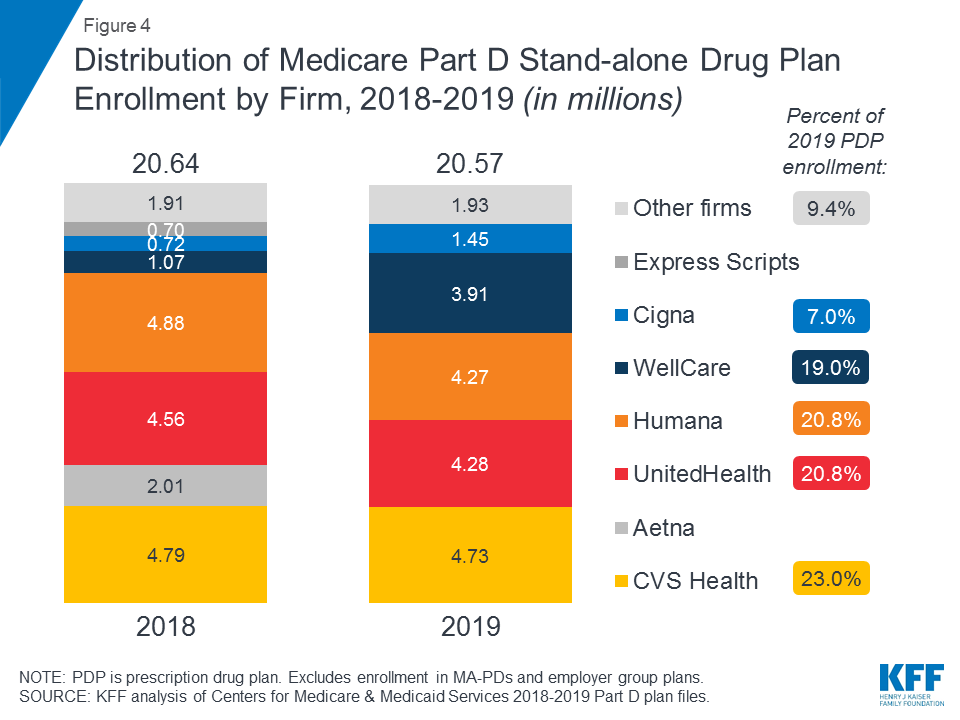
Blue cross blue shield prior authorization list. A few plans may continue to require prior authorization for mental health services. Forms and additional information can be downloaded on the CVS Caremark website. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
Diagnostic Imaging Prior Review Code List Prior review prior plan approval prior authorization prospective review or certification is the process Blue Cross NC uses to review the provision of certain behavioral health medical services and medications against health care management guidelines prior to the services being provided. Outpatient Prior Authorization CPT Code List 072 Prior Authorization Quick Tips. The list below includes specific equipment services drugs and procedures requiring review andor supplemental documentation prior to payment authorization.
When prior authorization is required you can contact us to make this request. Reviewed on a monthly basis to determine if updates are necessary based on services and procedures that. The list below is a standard precertification list.
Some services require prior authorization preauthorization before they are performed. Prior authorization sometimes called preauthorization or pre-certification is a pre-service utilization management review. Obtaining a prior authorization helps us pay claims faster with no denied charges or unexpected costs to our members.
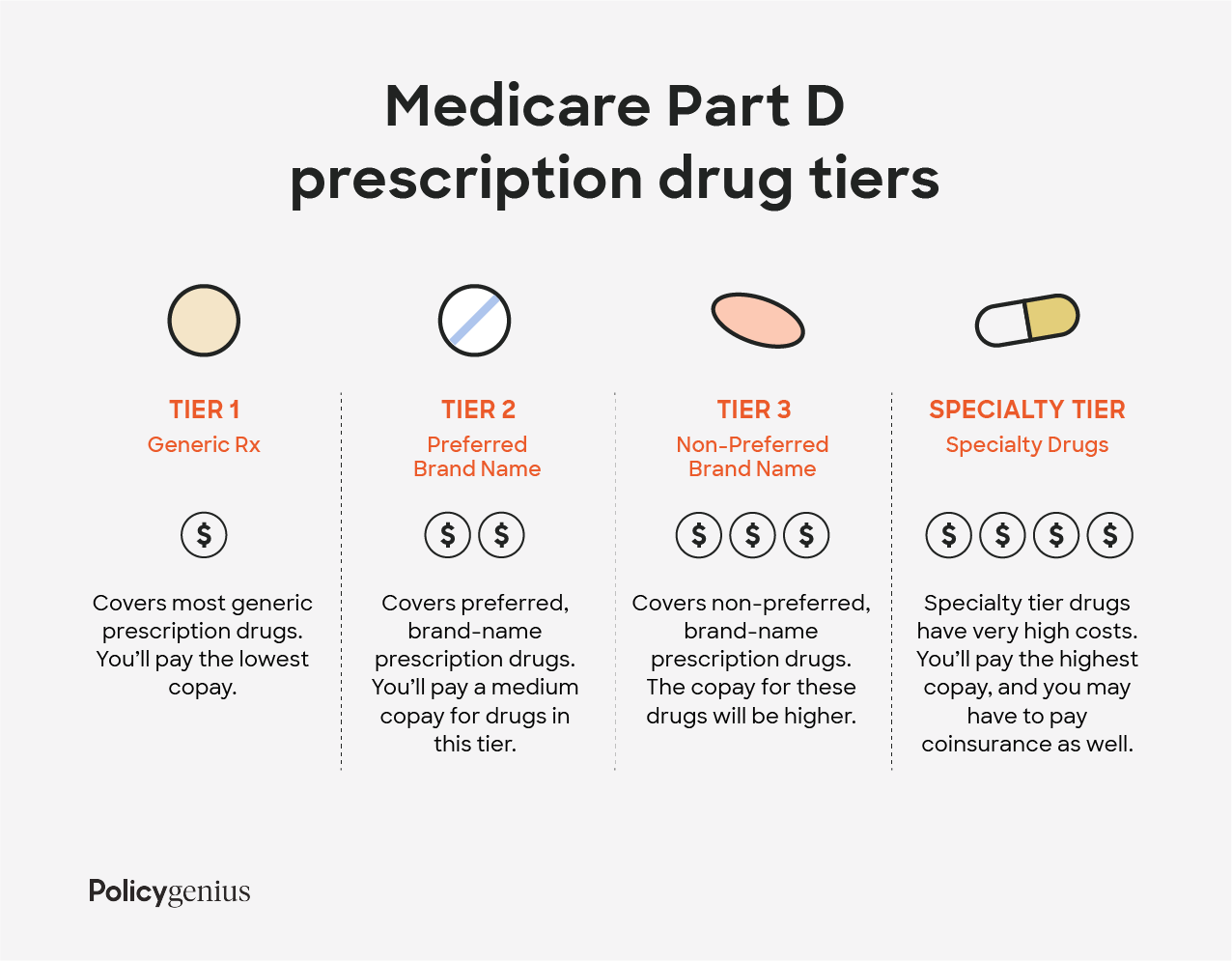
Urgentemergency admissions do not require prior authorization. BCBSNM requires preauthorization through eviCore for the services listed below for the following benefit plans. The Prior authorization list is a list of designated medical and surgical services and select prescription Drugs that require prior authorization under the medical benefit.
Medical Technology Assessment Non-Covered Services List 400. See the lists below for more details and our Blue Cross customer service is also available to help you. This list will be updated no more than twice a calendar year.
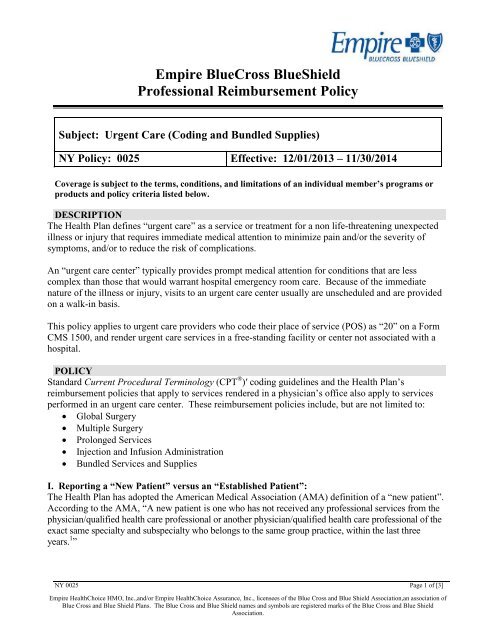
Blue Cross Medicare Advantage HMO-POS SM effective 06012017. Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization for your patients when its required. Blue Cross Medicare Advantage HMO SM effective 06012017.
Contact Companion Benefits Alternatives CBA to verify by calling 800-868-1032. Your doctor prescribes it in a medically appropriate way. Below is the list of specific services in these categories that require precertification.
Preauthorization Requirements for Blue Cross Medicare Advantage members. Advertentie Compare 50 Global Health Insurance Plans for Expats living abroad. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
Get a Free Quote. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. Assisted reproductive technology for GIFT ZIFT ICSI and IVF.
Some services may require a prior authorization to continue receiving the service after a set number of visits such as acupuncture and home health visits. These lists are not exhaustive. You should check this list prior to obtaining any outpatient hospital services physician services and other covered services.
For some services listed in our medical policies we require prior authorization. Prior authorization is required for some membersservicesdrugs before services are rendered to confirm medical necessity. You can see the full list of prescription drugs that need to be approved on the CVS Caremark website.
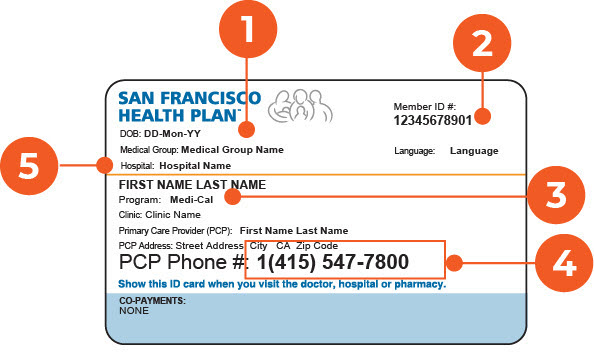
Your doctor can submit prior approval electronically by fax or by mail. Provider Preauthorization and Precertification Requirements - Blue Cross PPO and Medicare Plus Blue SM PPO PDF Northwood DMEPOS Management Program FAQ PDF Northwood DMEPOS Management Program Procedure Codes Requiring Prior Authorization PDF Patient eligibility precertification and preauthorization contacts. Some benefit plans have variations to the list.
CBA is a separate company that administers mental health and substance abuse benefits on behalf of BlueCross BlueShield of South Carolina and BlueChoice HealthPlan. It includes a complete list of services procedures and equipment that require pre-service review or have a Wellmark medical policy. 1 2021 Blue Cross and Blue Shield of Texas BCBSTX will update its list of Current Procedural Terminology CPT codes requiring prior authorization to comply with changes as a result of new replaced or removed codes implemented by the American Medical Association AMA and BCBSTX Utilization Management updates.
Advertentie Compare 50 Global Health Insurance Plans for Expats living abroad.