Orders must be submitted by 1159 pm. Llame a OTC Health Solutions para obtener ayuda al 1-866-528-4679 TTY.
 Medicare Over The Counter Drug Benefit Promedica Medicare Plan
Medicare Over The Counter Drug Benefit Promedica Medicare Plan
We experience high call volume the first and last weeks of the month.
Cvs otc health solutions. Call OTC Health Solutions OTCHS using the phone number listed above. If you receive a damaged item please call OTC Health Solutions at 1-833-331-1573 within 30 days after receiving your order. You can obtain your OTC items at select approved participating OTCHS-enabled CVS Pharmacy or Navarro stores.
To find your nearest location go to. Your OTCHS order can be placed at any time during the month. You will receive your order within 7-10 business days.
Once the ordering process begins you may order 15 items or less. Call OTC Health Solutions OTCHS using the phone number on file. 1-877-672-2688 2021 OTC Health Solutions.
How to use your OTC Health Solutions benefits in store. You can obtain your OTC items at select approved participating OTCHS-enabled CVS Pharmacy or Navarro stores. Products may be purchased at a local retail CVS pharmacy.
Once the system locates your account you will be asked to input your date of birth in MMDD format. Youll receive our OTC Catalog in the mail to do your shopping. Once the ordering process begins you may order 15 items or less.
Consult your OTC catalog. Address on the account. Once the system locates your account you will be asked to input your date of birth in MMDD format.
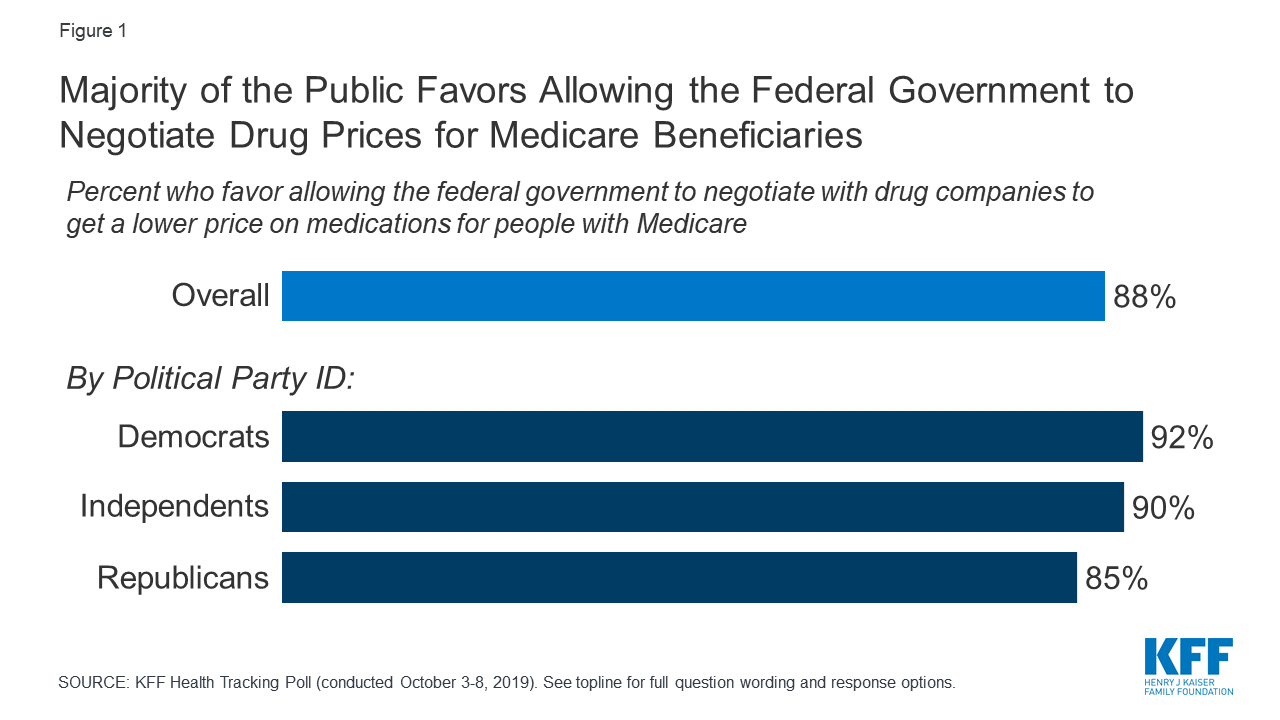
Many Premera Blue Cross Medicare Advantage MA plans have an over-the-counter OTC benefit of 50 per quarter for OTC health and wellness products. Clover Health presently works with OTC Health Solutions to enable members to make the most of their OTC benefit. Monday to Friday 900 am.
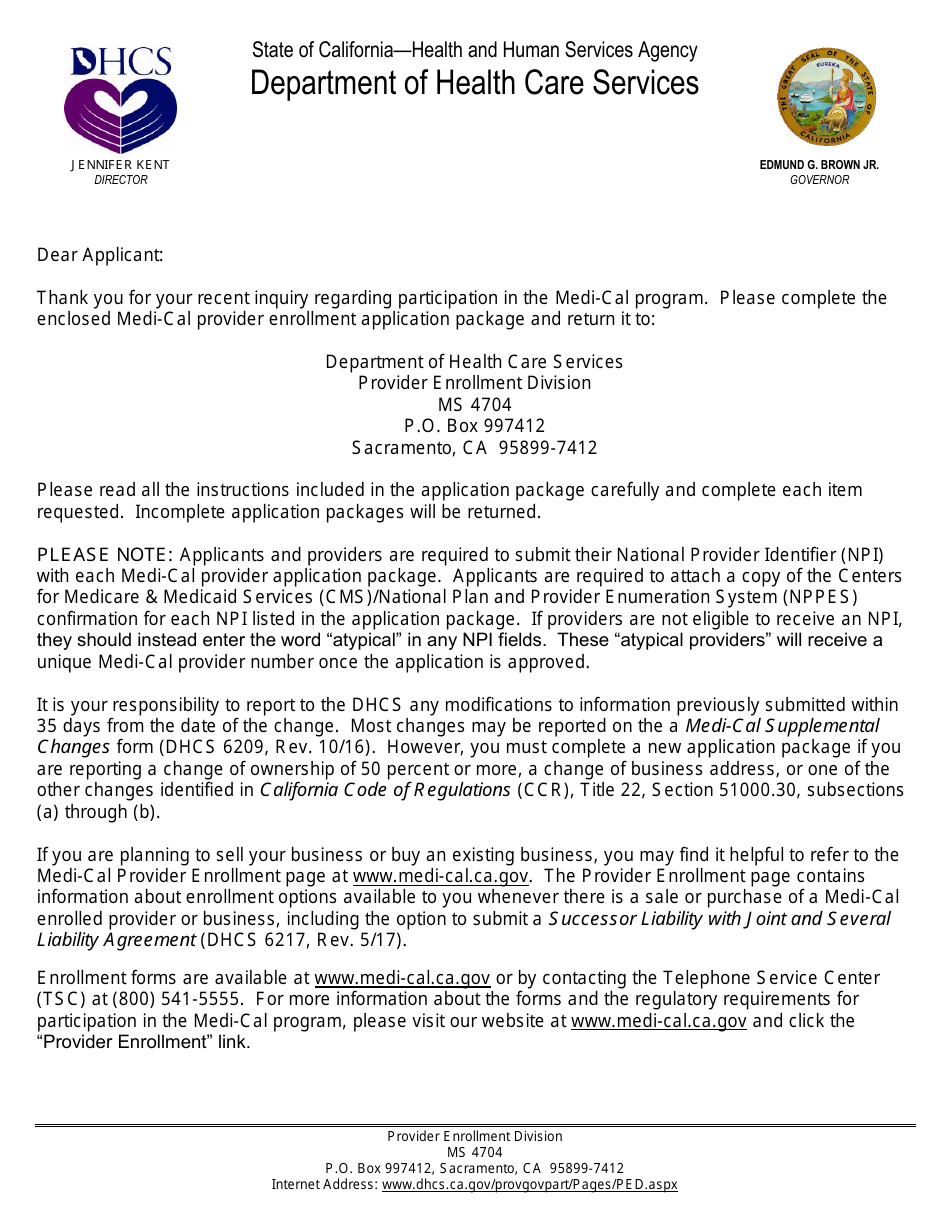
Please contact OTC Health Solutions customer service at 1-888-628-2770 and for TTYTTD assistance please dial 1-877-672-2688. Go to any select approved participating OTCHS. Our over-the-counter OTC benefit is in partnership with CVS Caremark.
Search the worlds information including webpages images videos and more. Identify approved items in the catalog. Orders must be submitted by 1159 pm.
To find a full list of stores. Its included with our Total Health Classic and Core Plus plans and our Alpine PeakRx SoundRx and CharterRx plans. OTC Health solutions has an online program that makes it achievable for millions of involved members to purchase items effortlessly.
Consult your OTC catalog. Use the store locator on. 1-877-672-2688 2021 OTC Health Solutions.
Did you know your plan covers some over-the-counter OTC purchases. Help your clients take advantage of this benefit during COVID-19. Identify approved items in the catalog.
Call OTC Health Solutions for help at 1-866-298-0578TTY. Google has many special features to help you find exactly what youre looking for. 1-877-672-2688 2021 OTC Health Solutions.
How to use your OTC Health Solutions benefits in-store. 1-877-672-2688 2021 OTC Health Solutions. How to use your OTC Health Solutions benefits in-store.
1-877-672-2688 2021 OTC Health Solutions. Call OTC Health Solutions for help at 1-888-628-2770TTY. Go to any select approved participating OTCHS.
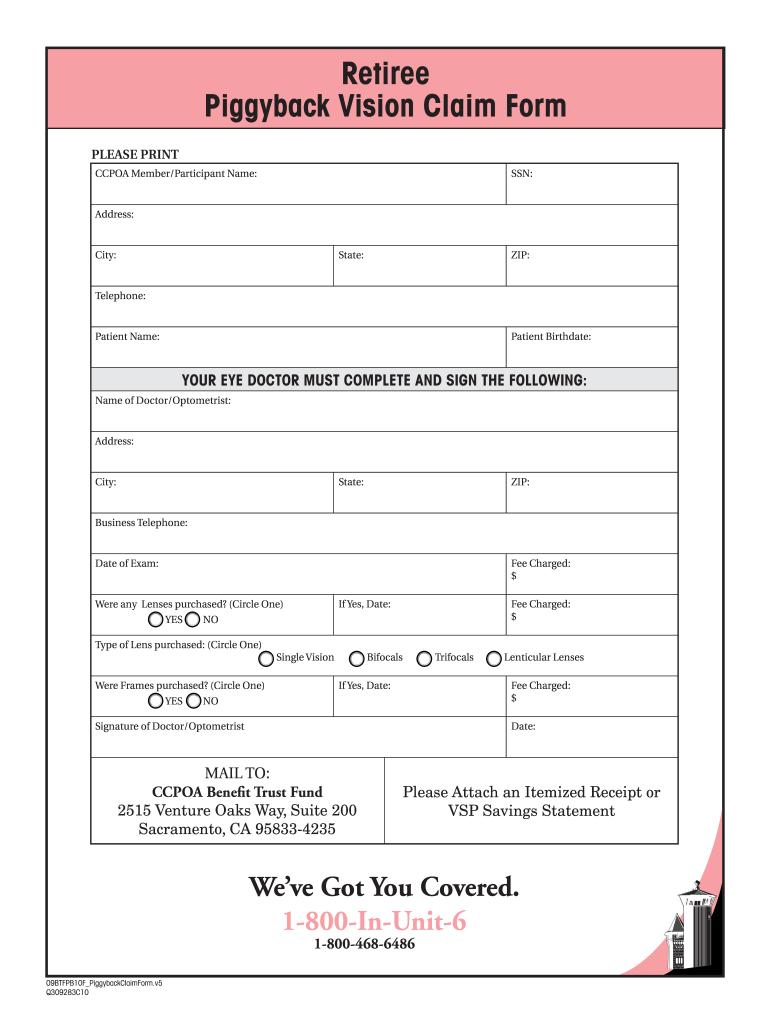
To find your nearest location go to. Call OTC Health Solutions for help at 1-833-331-1573 TTY. Members receive a quarterly amount to purchase from over 300 CVS-brand over-the-counter products including.
Our benefit offers you an easy way to shop CVS-branded over-the-counter health and wellness products and have them shipped directly to your home. All these may be purchased at a number of participating CVS pharmacies. Look for the blue labels identifying eligible products.
Rewards for CVS Pharmacy over-the-counter OTC their members get a fixed allowance quarterly which may be used to order from a vast selection of OTC health-related products like personal care items and cold remedies. Call OTC Health Solutions for help at 1-833-331-1573 TTY. 1-877-672-2688 2021 OTC Health Solutions.
To be processed that day. The account authentication process will start and the system will verify the name and address on the account. Go to any OTCHS-enabled CVS Pharmacy or CVS Pharmacy y mas store.
Consult your health plan catalog. Identify approved items in the catalog. Call OTC Health Solutions for help at 1-888-628-2770 TTY.
To be processed that day. Your OTCHS order can be placed at any time during the month. Todos los derechos reservados.
Please introduce the numerical portion of the item code.