Trying working out at home or going to reasonably priced gyms like 24 Hour Fitness. If you are interested in a Medicare gym membership make sure the Medicare Advantage plan you choose includes this benefit.
 Does Health Insurance Cover Gym Memberships Lovetoknow
Does Health Insurance Cover Gym Memberships Lovetoknow
The table below displays a snapshot of Bupas extras only health insurance policies on Canstars database sorted by Star Rating.

Does insurance cover gym membership. Beneficiaries can enroll in Silver Sneakers to get membership to a fitness center near them. I feel like Im selling health club memberships. Gym memberships group exercise classes nutrition programs personal training and home exercise equipment can all be eligible for reimbursement.
People that sign up for an Advantage plan must pay the Part B premium and any plan costs. You may not be aware but some insurance policies specifically extras policies cover memberships to health and lifestyle programs such as. The benefits are pretty obvious.
Silver Sneakers is offered through certain insurance companies that cover Medicare beneficiaries. However some other parts of Medicare may offer a benefit for. However they often may give you a limited amount of money 250 for example towards the cost of it.
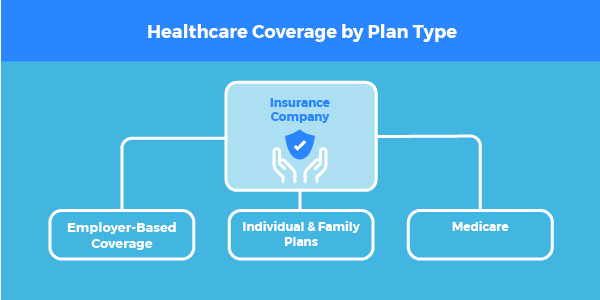
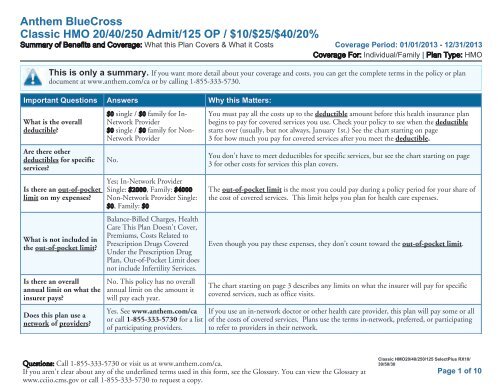
Whether your health insurance will cover or pay for a gym membership depends on your carrier Blue Cross Blue Shield Aetna Oxford Cigna and more and your individual plan. A gym membership as a health insurance benefit is a bit of a double-edged sword. However there are some Medicare Advantage and Medicare Supplement plans that offer gym reimbursements.
Exercise class memberships eg. Some plans may offer a discount on memberships of facilities the carrier has an associationcontract with. If your gym plan takes 30 a month out of your checking account a half-off discount will save you 15 each month.
Most providers however will offer you a stipend or reimbursement for fitness costs usually around 200 per year or so plus other benefits and discounts. Contrary to popular opinion your health insurance provider has a vested interest in you staying healthy. Original Medicare Medicare Part A and Part B is administered by the federal government and does not typically include coverage for gym memberships.
How do you qualify for Silver Sneakers. Does Medicare Cover Gym Memberships. Its amazing to me that gym membership add ons become more important than the supplement or Med C coverage itself.
Some work with specific gyms to give you a discount or even a free membership while others will offer your a set amount in reimbursement. In general health insurance companies will not pay for your gym membership directly. They are required to cover the same benefits as Original Medicare but they are free to also offer some additional benefits.
If you have one of these call your plan to see if it covers gym memberships or fitness programs. If youre passionate about both your health and finances the benefits of taking out a health insurance policy that covers gym membership could be multifold. As a result many insurers cover gym memberships in one way or another.
Advantage plans can offer extra benefits that arent available through Medicare. Medicare gym membership can also be a benefit with a Medicare Advantage plan. If you have one of those plans you have it at no additional cost.
The answer is they will often pay a little towards the cost of your membership. Gym memberships or fitness programs may be part of the extra coverage offered by Medicare Advantage Plans other Medicare health plans or Medicare Supplement Insurance Medigap plans. Ridiculous that this even enters our conversations repeatedly as insurance agents.
Does your health insurance cover a gym membership. Many health insurance plans include discounts on specific health club memberships that range from about 10 to 50 off the normal price. Monthly membership discount N7156 E Plaza Dr.
An individual health insurance plan is generally not going to pay for your gym membership. Original Medicare does not provide coverage for gym memberships or fitness classes. No words on whether thats per month per year or something else.
Some health insurance policies can even reward healthier behaviour by offering lower premiums to those who are keeping fit and making conscious lifestyle decisions. According to Aetna you and your partner can be reimbursed for up to 150. Medicare doesnt cover the costs of fitness programs and gym memberships although some advantage plan includes a gym membership.
It is important to note this does not cover 24-hour gyms gym membership for general fitness casual gym sessions or boot camp sports clothing or shoes or personal trainers. Does Medicare pay for a gym membership. If you want to try.
Access to a gym could keep. Medicare Advantage plans are provided by private insurance companies. Yoga swimming Pilates Skin cancer screenings.
Naturally many companies offer discounts or. If your insurer doesnt cover gym memberships that doesnt mean you cant get fit. However they may offer certain wellness programs for you to be active and continue your good health.